In Part 1 of ‘The Oxygenator Assessment’ we learnt what the oxygentor is. In Part 2 we are going to look at the 6 big issues that need to be covered from an airway assessment perspective:
- The atmosphere
- Mask ventilation
- Laryngoscopy/intubation → infraglottic
- Rescue airway → supra/extraglottic
- Surgical airway
- Lung compliance
- The Atmosphere
I include this as part of the assessment as it is the primary determinant of the initial concentration of O2 you have at your disposal. It will be influenced by atmospheric pressure, fractional inspired O2, geographical location, the various O2 delivery interfaces available -or not- and the relative ability to adapt these factors acutely.
It requires no stretch of the imagination to realize that nasal prongs at 4 l/min may not deliver as much O2 as a 60% face mask, and a room air 21% O2 may need to be bumped up to 100% if respiratory failure is imminent. That too can be a problem if the interface for delivery of the O2 at best is a CPAP mask or can be adjusted to an endotracheal tube with a ventilator on standby.
The point is don’t neglect the environment in which you are delivering oxygen from. It is from here that all O2 flows. Prepare yourself to do rapid calculations of expected PI O2 at a given atmospheric level, calculate PAO2, paO2, and A-a gradients…and react to them if and when possible to improve O2 delivery.
- Mask Ventilation:
The mnemonics OBESE and MOANS can be used as predictors of difficult face mask ventilation:
OBESE
- OBESE
- Obese BMI >30 kg/m2
- Bearded
- Elderly >55
- Snorers /Sleep apnea patients
- Edentulous
MOANS
- Mask seal (beards, blood, discontinuous anatomy)
- Obesity, Obstruction (obese, pregnancy, angioedema, Ludwig’s angina, upper airway abscess, epiglottitis)
- Age- >55
- No teeth (leave dentures in place for mechanical ventilation!)
- Sleep apnea, Stiff lungs (COPD, asthma, ARDS)
- Laryngoscopy/Inubation:
The mnemonic LEMON is a useful predictor of difficult laryngoscopy/intubation:
LEMON
- Look externally (common sense, trauma, le forte fractures, disrupted anatomy, abnormal anatomy of mouth, tongue, jaw, teeth, agitated patient, big breasts)
- Evaluate (use the 3-3-2 rule)
- Mallampati Score (grades 1-4)
- Obesity (poor views of glottis with obesity), Obstruction (4 signs of upper airway obstruction = stridor, muffled voice, difficulty swallowing secretions, sensation of dyspnea)
- Neck mobility (trauma, cervical spine disease, rheumatoid disease, spondylitis, trisomy 21, halo devices, previous fusions)
Some elaboration is required to highlight the LEMON mnemonic. I must also reiterate that this is not a full treatment of the issue. Instead it is a drop down box for you in the early mornings and weekends and on those late, tired days on call.
The ability to bite the upper lip with bottom set of teeth tells us a fair amount about the ability to jaw thrust, malocclusion of dentition, overbite, under bite, big jaws e.g. GH excess. You either can bite above vermillion border, reach the border, or cant. Difficulty in intubation increases with decreasing upper lip biting ability
Atlanto axial and occipital movement should also be considered. RECALL WE MUST ALIGN THREE AXIS TO INTUBATE! Any hindrance anatomically to straightening those axis into one line makes bending any rigid tube and scope impossible.
The Mallampati classification comprises a visual assessment of the distance from the tongue base to the roof of the mouth. A high Mallampati score (class 3 or 4) is associated with more difficult laryngoscopy and intubation. The patient should be assessed sitting upright with no phonation. They should open their mouth and protrude the tongue as much as is possible. It is scored depending upon what is visible:
- Class I: soft palate, uvula, fauces, pillars visible
- Class II: soft palate, uvula, fauces visible
- Class III: soft palate, base of uvula visible
- Class IV: only hard palate visible
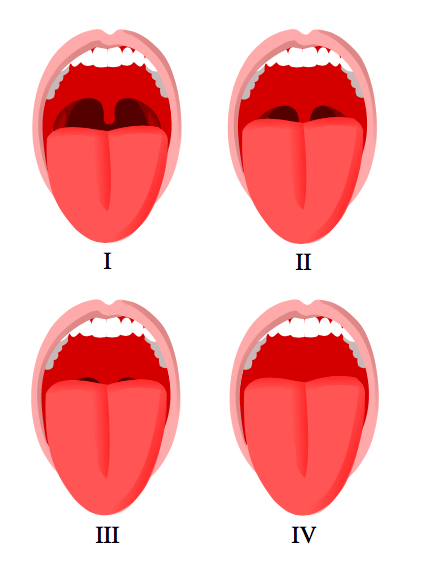 The Mallampati classification sourced from Wikipedia
The Mallampati classification sourced from Wikipedia
Courtesy of Jordi March i Nogué CC BY-SA 3.0
The 3-3-2 rule looks at the space from chin to thyroid. It assesses how much space is available for manipulation, and how rigid, stiff or compliant is it. Normal mouth opening is three of the patient’s fingerbreadths and a mouth that can open that far has good temporomandibular joint mobility. A normal mandible dimension will also allow three fingerbreadths between the mentum and the hyoid bone. If it is shorter than this intubation will become more difficult. Finally the notch of the thyroid cartilage should be two fingerbreadths below the hyoid bone.
The following are useful numbers to remember for predicting problems with intubation:
- Mallampati 3 or 4
- Neck circumference >40 cm
- BMI > 30
- Thyromental distance <6.5 cm
- Interincisor gap < 4 cm
- Extraglottic devices – rescue airways:
Here we are talking about guedel airways, nasopharyngeal airways, and laryngeal mask airways. Remember you cannot put an oropharyngeal airway in an awake patient with an intact gag and in these circumstances you should use a nasopharyngeal airway. Oropharyngeal airways should be reserved for obtunded, unconscious patients.
The mnemonic RODS is a useful predictor of difficult extraglottic device insertion:
RODS
- Restricted mouth opening
- Obstruction anywhere from mouth to larynx
- Disrupted/ distorted anatomy
- Stiff lung/stiff spine
It is important to note that these are not definitive airways. They don’t protect the patient from aspiration, they rely on permissive hypercapnia, and are not a perfect seal. They are rescue devices. Know their pitfalls.
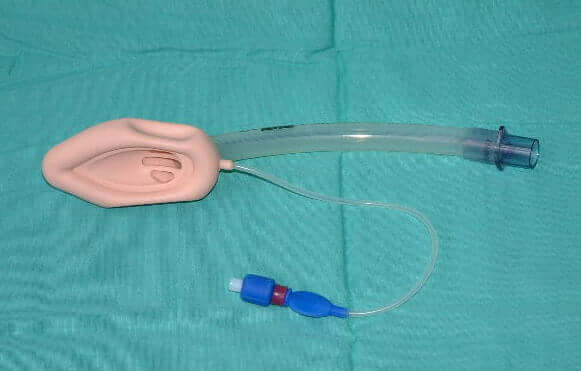
Laryngeal mask airway- image sourced from Wikipedia
Courtesy of Prof. Chris Wheatley CC BY-SA 3.0
- Surgical airway:
The last stop for us is cutting an airway. It is the last attempt at salvaging life, at rescuing a situation gone too far. Ideally a surgeon should be available.
The mnemonic SHORT is a useful predictor of difficult cricothyroidotomy:
SHORT
- Surgery or other airway obstruction
- Hematoma includes abscess and infection
- Obesity – where is everything and vascularity
- Radiation/ Burns distortion
- Tumor
- Lung compliance:
The final aspect is of vital importance. It encompasses all anatomy, from chest wall to tracheobronchial tree and alveoli. It is not in the scope of this to discuss the innumerable issues here, but in summary, any pathology producing restrictive/obstructive or combination disease of the airway and its anatomy will make pressure changes to deliver a given volume of flow that much greater.
Thank you, I hope you look at the oxygenator with new, excited eyes and preempt problems in all patients. They are all potentially an airway waiting to be secured.
Cheers.
Medical Exam Prep would like to thank Dr. Clem Lonnigen Jolly for contributing this post.
About Dr. Clem Lonnigen Jolly
Dr. Clem Lonnigen Jolly is an Anaesthetist working at the Ethekwini Hospital and Heart Centre in KwaZulu-Natal, South Africa
Header image used on licence from Shutterstock






Great re- enforcement!
Thank you!!!.