Dealing with a patient with abnormal liver function tests (LFTs) in the primary care setting is an extremely common clinical scenario. Approximately 20% of all LFTs are abnormal, of which less than 10% can be explained by existing disease.
LFTs are not specific to precise systems or particular disease processes, but abnormalities may indicate significant or serious disease. Abnormal LFTs are also frequently inadequately investigated, which can lead to missed diagnoses or a lost opportunity for early detection of liver disease. Recognising specific patterns of abnormalities within the tests can help to determine the origin of the issue, particularly when this is then combined with a thorough clinical assessment.
The following guidance is taken from the 2017 British Society of Gastroenterology guidelines on the management of abnormal liver function tests.
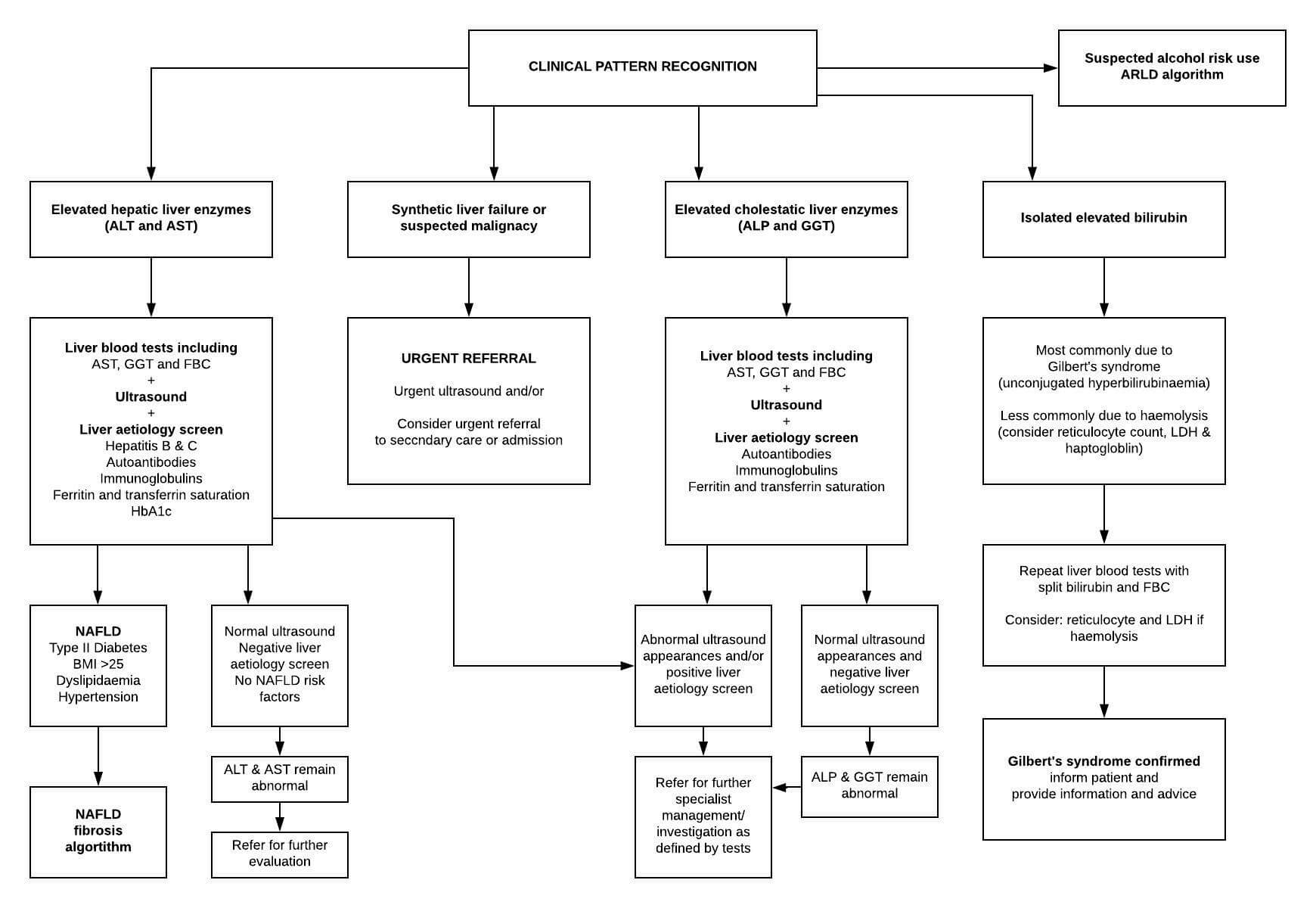
Elevated hepatic liver enzymes (ALT and AST)
In patients with elevated hepatic liver enzymes (ALT and AST), it is recommended that liver blood tests are checked if not already performed (to include AST, gamma GT and a full blood count). An ultrasound and a liver aetiology screen should also be performed.
The liver aetiology screen should include:
- Hepatitis B and C serology
- Anti-mitochondrial, anti-smooth muscle and antinuclear antibodies
- Serum immunoglobulins
- Ferritin and transferrin saturation
The patient should also be assessed for non-alcoholic fatty liver disease (NAFLD) risk factors, e.g. type II diabetes mellitus, BMI >25, dyslipidaemia and hypertension. If NAFLD is suggested, either by the presence of risk factors and a negative liver screen or by the ultrasound scan, then the patient should be managed according to the NAFLD algorithm (see below).
If the ultrasound scan is abnormal and/or there is a positive liver aetiology screen, then the patient should be referred for further specialist management/investigation as defined by the test results.
If the ultrasound scan is normal, there is a negative liver aetiology screen, and there are no NAFLD risk factors, the patient should be monitored and the ALT and AST re-checked. If the hepatic liver enzymes remain elevated, then the patient should be referred for further evaluation.
Elevated cholestatic liver enzymes (ALP and GGT)
In patients with isolated elevated cholestatic liver enzymes (ALP and gamma GT), it is recommended that liver blood tests are checked if not already performed. An ultrasound and a liver aetiology screen should also be performed. The presence of an elevated gamma GT can help to determine a liver cause of a raised ALP, rather than a bony cause or vitamin D deficiency.
If the ultrasound scan is abnormal and/or there is a positive liver aetiology screen, then the patient should be referred for further specialist management/investigation as defined by the test results.
If the ultrasound scan is normal and there is a negative liver aetiology screen, the patient should be monitored and the ALP and gamma GT re-checked. If these remain abnormal, then the patient should be referred for further evaluation.
Isolated elevated bilirubin
An isolated elevated bilirubin level when the other liver function tests are normal is most commonly caused by Gilbert’s syndrome. This is usually an autosomal recessive disorder and is a common cause of unconjugated hyperbilirubinaemia, affecting 5-8% of the population.
Liver function tests should be repeated with a split bilirubin and a full blood count on a fasted sample. Total bilirubin should rise further in Gilbert’s syndrome due to the indirect component, and there should be no anaemia present. If Gilbert’s syndrome is confirmed the patient can be informed and counselled about the diagnosis.
If there is anaemia present, haemolysis should be considered, and the reticulocyte count, LDH and haptoglobin levels checked.
Patients with synthetic liver failure
If the patient has evidence of synthetic liver failure, e.g. jaundice, low albumin and/or a prolonged INR, or a suspected malignancy, e.g. weight loss and/or marked cholestasis, then an urgent referral should be made, either for an ultrasound scan or direct to secondary care.
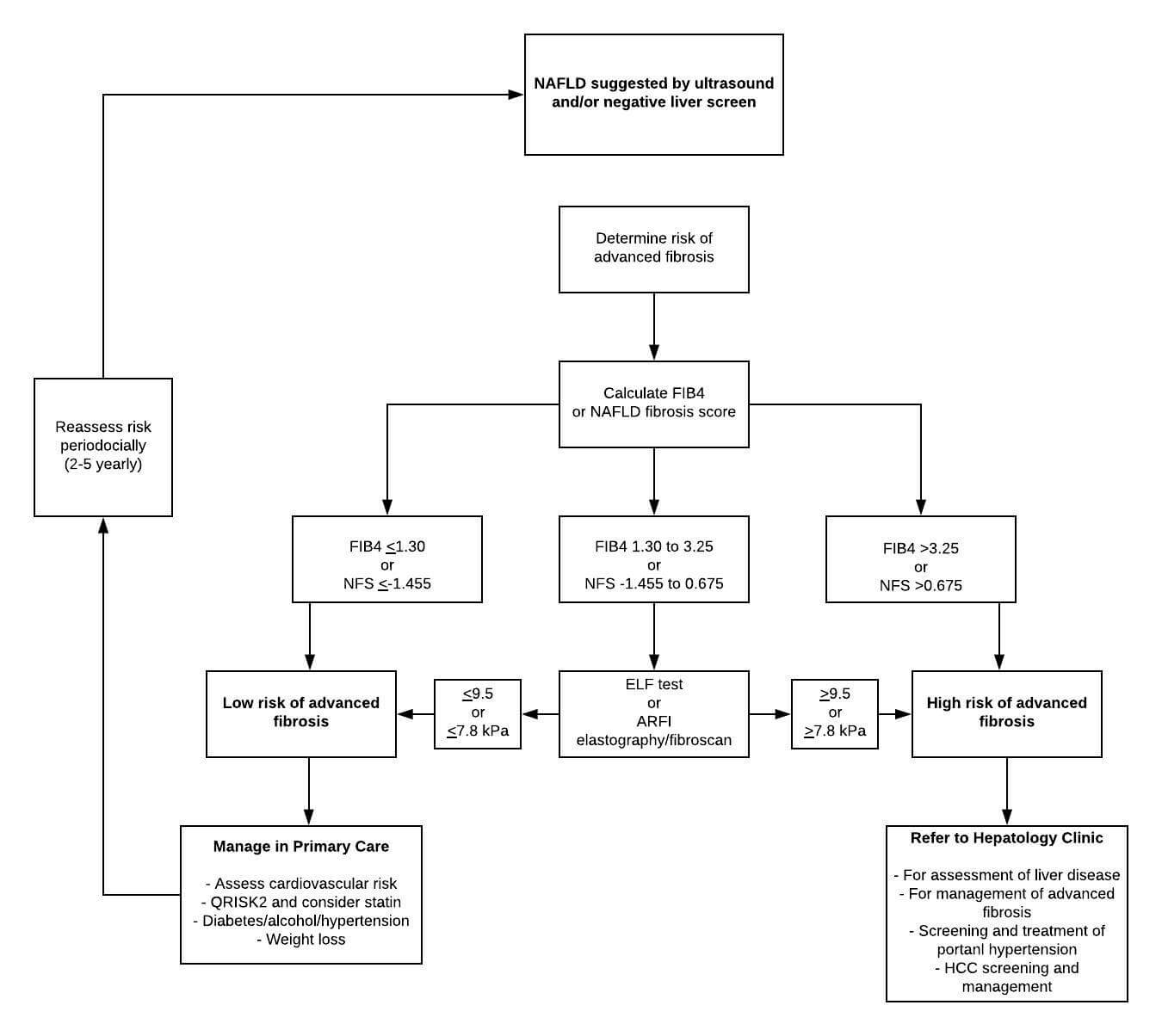
Non-alcoholic fatty liver disease (NAFLD) algorithm
In the Western world, alcohol is the most common cause of fatty liver (alcoholic fatty liver disease). Other causes of fatty liver include:
- Malnutrition (of protein)
- Diabetes mellitus
- Pregnancy
- Obesity
- Hepatotoxins
Non-alcoholic fatty liver disease (NAFLD) is most commonly caused by obesity in the western world. Patients classically have a raised BMI associated with truncal obesity. Most patients also go on to develop impaired glucose tolerance or diabetes.
In alcoholic fatty liver disease the typical pattern of AST: ALT ration is >1 and the MCV is usually also raised. In NAFLD, the usual pattern is AST: ALT < 1.
In patients with NAFLD, discovered either as an incidental finding on an ultrasound scan or via investigation of abnormal liver function tests, NICE currently recommends the enhanced liver fibrosis (ELF) test. This is an accurate blood test for assessing fibrosis which makes the need for liver biopsy virtually redundant. It is, however, expensive, and not widely available at present.
The BSG guidelines also recommend acoustic radiation force impulse (ARFI) imaging as an alternative. This is an ultrasound-based diagnostic technique that, evaluating the wave propagation speed, allows the assessment of the tissue stiffness. It is a non-invasive, sensitive and accurate tool for the assessment of liver fibrosis and the discrimination between cirrhotic and non-cirrhotic liver.
Depending upon the results of these investigations, the patient can either be managed in primary care or referred to a hepatology clinic, as shown in the algorithm below:
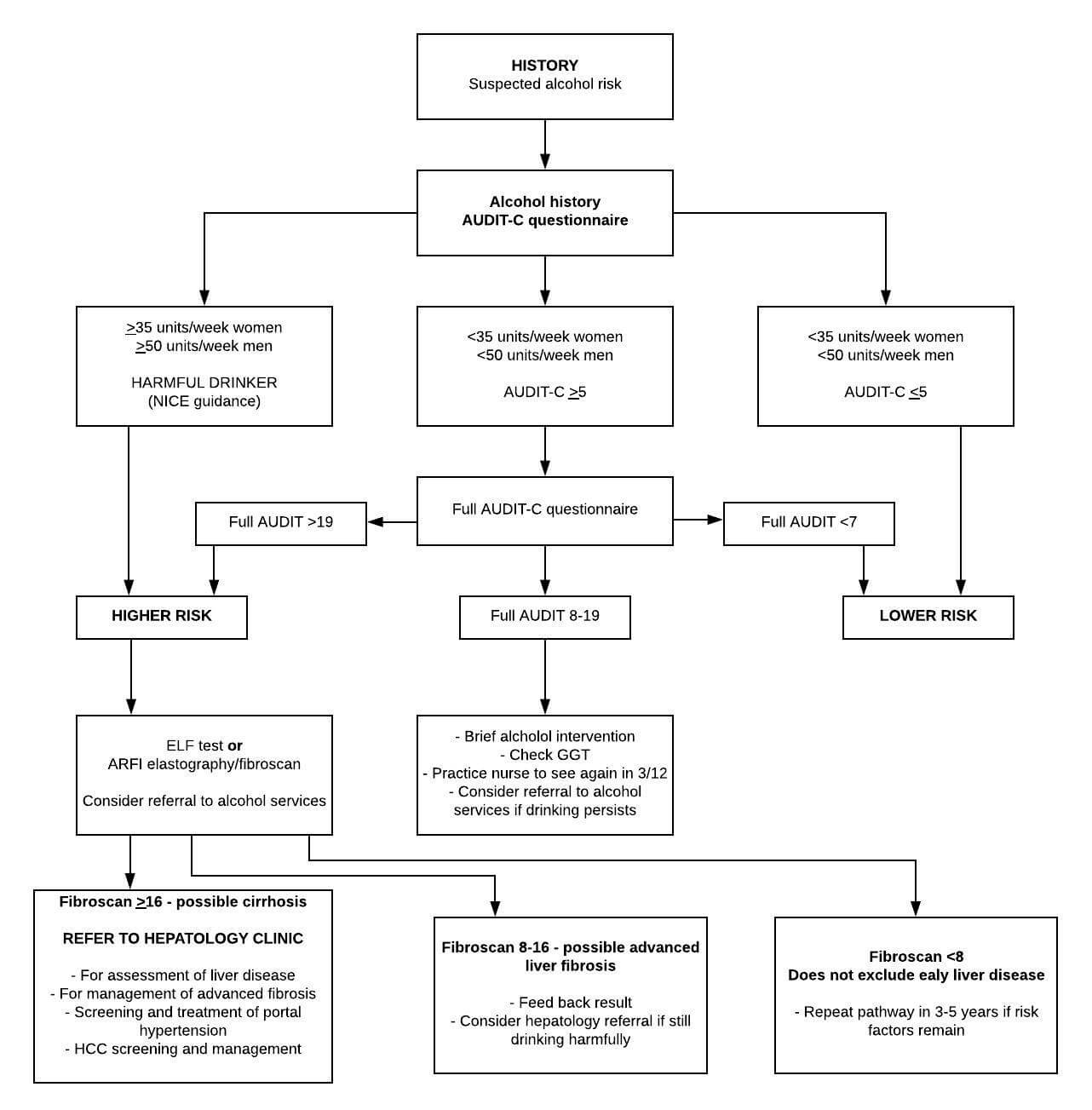
Patients with suspected alcohol risk
In patients in whom alcohol is suspected to be the main injurious factor, the extent of consumption influences early decision-making. For those drinking at harmful levels, ≥35 units/week women and ≥50 units/week men, an assessment of liver fibrosis is the critical next step.
For other patients, administration of the AUDIT-C questionnaire alongside brief intervention is recommended initially. For patients who continue to drink at hazardous levels, consideration should be given to assessment as for the higher-risk category according to liver fibrosis evaluation. This is particularly important for those with a GGT of >100 U/L.
Further reading:
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this article.






This is refreshing especially for the young doctors