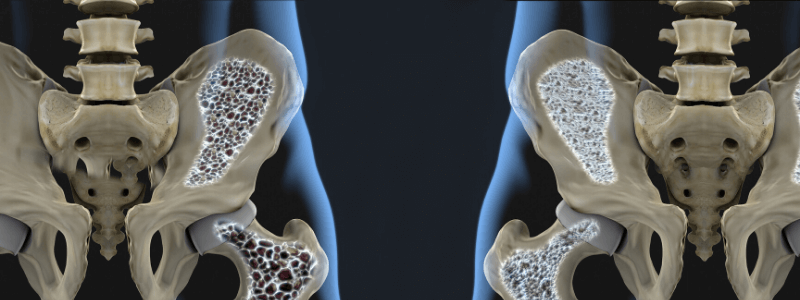
Osteoporosis is a progressive systemic skeletal disease characterised by low bone mass and structural deterioration of bone tissue. Consequently, bone fragility is increased and there is increased susceptibility to fracture.
Osteoporotic fragility fractures are fractures that result from mechanical forces that would not ordinarily result in a fracture (low-level, or ‘low-energy’ trauma). The World Health Organization (WHO) has quantified this as forces equivalent to a fall from a standing height or less. Fragility fractures occur most commonly in the spine (vertebrae), hip (proximal femur) and wrist (distal radius).
Epidemiology
Osteoporosis is the most common bone disease and is an enormous healthcare burden. It is estimated that over 2 million women in the UK have osteoporosis. Approximately a third of all women and a fifth of all men will suffer an osteoporotic fragility fracture at some point in their lifetime.
Bone loss increases in both men and women with increasing age and increases dramatically after the menopause in women. Consequently, the prevalence of osteoporosis increases progressively with advancing age, from 2% at 50 years to more than 25% at 80 years in women.
The risk factors for osteoporosis include the following:
- Increasing age
- Female gender
- Premature menopause in women
- Low body mass index (<20 in women and <25 in men)
- Use of oral or systemic corticosteroids
- Family history of osteoporosis
- Previous fracture history
- Current smokers
- Excessive alcohol intake
- Low calcium and vitamin-D intake
Important definitions
Bone mineral density (BMD) is usually expressed in relation to a reference population in standard deviation (SD). This can be expressed as either a:
- T score – when bone density is compared to a young healthy population, or
- Z score – when bone density is compared to the normal at that age.
The WHO have established the following definitions on the basis of BMD assessment:
- Normal: hip BMD greater than the lower limit of normal which is taken as 1 SD below the young adult reference mean (T score ≥ -1)
- Low bone mass (osteopenia): hip BMD between 1 and 2.5 SD below the young adult reference mean (T score less than -1 but above -2.5)
- Osteoporosis: hip BMD 2.5 SD or more below the young adult reference mean (T score ≤-2.5)
- Severe osteoporosis: hip BMD 2.5 SD or more below the young adult reference mean in the presence of one or more fragility fractures (T score ≤-2.5 PLUS fracture).
Bone density can be measured by a number of investigative tests, but the one most commonly used is dual-energy X-ray absorptiometry (abbreviated to DEXA or DXA).
Targeting risk assessment
The current NICE guidelines recommend that clinicians should consider the assessment of fracture risk in the following groups:
- In all women aged 65 years and over and all men aged 75 years and over
- In women aged under 65 years and men aged under 75 years in the presence of risk factors, for example:
- Previous fragility fracture
- Current use or frequent recent use of oral or systemic glucocorticoids
- History of falls
- Family history of hip fracture
- Other causes of secondary osteoporosis*
- Low body mass index (BMI) (<18.5 kg/m2)
- Smoking
- Alcohol intake of >14 units per week for women and >21 units per week for men.
Fracture risk should not be routinely assessed in people under the age of 50 years unless they have a major risk factor for osteoporosis, such as current or frequent recent use of oral or systemic corticosteroids, untreated premature menopause or a previous fragility fracture.
It is very unusual to need to assess the risk of fracture in patients under the age of 40; however, NICE recommend that is should be assessed if any of the following major risk factors are present:
- History of multiple fragility fractures,
- A major osteoporotic fracture
- Current or recent use of high-dose oral or high-dose systemic corticosteroids (e.g. >7.5 mg prednisolone or equivalent daily for >3 months).
Secondary causes of osteoporosis*
The secondary causes of osteoporosis are summarised in the table below:
| System involved | Examples |
|---|---|
| Endocrine | Hypogonadism Hyperthyroidism Hyperparathyroidism Hyperprolactinaemia Cushing’s disease Diabetes |
| Gastrointestinal | Coeliac disease Inflammatory bowel disease Chronic liver disease Chronic pancreatitis Other malabsorption syndromes |
| Rheumatological | Rheumatoid arthritis Other inflammatory arthropathies |
| Haematological | Multiple myeloma Haemoglobinopathies Systemic macrocytosis |
| Respiratory | Cystic fibrosis Chronic obstructive pulmonary disease |
| Metabolic | Homocystinuria |
| Renal | Chronic renal disease |
Methods of risk assessment
NICE recommend the use of either of the following tools to assess the risk of fragility fracture in at-risk groups:
- FRAX
- Qfracture
Both of these scores estimate a 10-year predicted absolute risk of fracture. The estimated absolute risk of fracture in people aged over 80 years should be interpreted with caution, because predicted 10-year fracture risk may underestimate their short-term fracture risk. Above the upper age limits defined by these tools, people should be assumed to be at high risk.
FRAX
The WHOs Fracture Risk Assessment Tool (FRAX) can be used for people aged between 40 and 90 years, either with or without BMD values, as specified.
The FRAX tool incorporates the following clinical risk factors into its algorithm:
- Age
- Sex
- Weight
- Height
- Previous fracture
- Parental hip fracture
- Current smoking
- Corticosteroid usage
- Rheumatoid arthritis
- Secondary osteoporosis
- Alcohol intake (≥3 units/day)
The FRAX tool calculates a 10-year probability of hip fracture and the 10-year probability of a major osteoporotic fracture (clinical spine, forearm, hip or humerus fracture). It can be used either with or without BMD results, and is often expressed as either ‘FRAX with BMD’ or ‘FRAX without BMD’.
Qfracture
The Qfracture tool was developed based on primary care populations in the UK and, therefore, may be more applicable to the UK population. It can be used for people aged between 30 and 84 years. BMD values cannot be incorporated into the risk algorithm. Unlike the FRAX tool, Qfracture can only be calculated without a BMD value.
The Qfracture tool incorporates the following clinical risk factors for both men and women:
- Age
- Sex
- Body mass index
- Smoking
- Alcohol intake
- History of falls
- Corticosteroid usage
- Tricyclic antidepressants usage
- Asthma
- Cardiovascular disease
- Chronic liver disease
- Rheumatoid arthritis
- Type 2 diabetes
The following additional factors are used in women only:
- Hormone replacement therapy usage
- Parental history of hip fracture
- Menopausal symptoms
- Gastrointestinal malabsorption (e.g. coeliac disease, inflammatory bowel disease)
- Endocrine disorders (e.g. hyperthyroidism, Cushing’s syndrome)
Recalculating fracture risk
NICE recommend that clinicians should consider recalculating the fracture risk in the future:
- If the original calculated risk was in the region of the intervention threshold for a proposed treatment and only after a minimum of 2 years,or
- When there has been a change in the person’s risk factors.
Further reading:
NICE guideline: Osteoporosis: assessing the risk of fragility fracture
NICE Clinical Knowledge Summary: Osteoporosis: assessing the risk of fragility fracture
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this article.