The latest guidance from NICE for the management of stroke was keen to highlight the fact that it is both preventable and treatable and not merely an inevitable consequence of ageing.
Stroke is defined by the World Health Organization as a clinical syndrome consisting of ‘rapidly developing clinical signs of focal (at times global) disturbance of cerebral function, lasting more than 24 hours or leading to death with no apparent cause other than that of vascular origin’.
A transient ischaemic attack (TIA) is defined as stroke symptoms and signs that resolve within 24 hours. The symptoms of a TIA usually resolve within minutes or a few hours at most, and anyone with continuing neurological signs when first assessed should be assumed to have had a stroke.
Most strokes are caused by a blockage cutting off the blood supply to the brain. These are referred to as ischemic strokes (approximately 85% of strokes). Strokes can, however, also be caused by bleeding in or around the brain. These are referred to as haemorrhagic strokes (approximately 15% of strokes).
Epidemiology
Stroke is a significant health problem in the UK. It is the third most common cause of death. The vast majority of patients that suffer a stroke are over the age of 65, but stroke can occur at any age.
Most people survive a first stroke but often have significant morbidity. Each year in England, around 110,000 people have a first or recurrent stroke, and a further 20,000 people have a TIA. Stroke accounts for more than 58,000 deaths yearly in England and Wales, representing around 10% of all deaths. Over 900,000 people in England are living with the effects of stroke, with half of these being dependent on other people for help with everyday activities.
The recognised risk factors for stroke and TIA include:
- Hypertension
- Smoking
- Diabetes mellitus
- Hyperlipidaemia
- Heart disease (valvular, ischaemic, atrial fibrillation)
- Peripheral vascular disease
- Polycythaemia
- Carotid artery occlusion
- Combined oral contraceptive pill usage
- Hyperlipidaemia
- Thrombophilias
The Cerebral Circulation
The brain receives a relatively large proportion of the body’s blood supply. Despite only accounting for approximately 2% of the total body weight, it receives a rate of cerebral blood flow of around 750 ml per minute, which is approximately 15-20% of the cardiac output. The arterial supply is divided into anterior and posterior segments, with the anterior segment receiving its arterial supply from the internal carotid arteries and the posterior segment and brainstem receiving its blood supply from the vertebral arteries.
The two anterior cerebral arteries arise from the internal carotid arteries. They are responsible for the arterial supply to most midline portions of the frontal lobes and superior medial parietal lobes.
The two middle cerebral arteries also arise from the internal carotid arteries. They are responsible for the arterial supply to the anterior temporal lobes and the insular cortices.
The posterior cerebral arteries are formed by the bifurcation of the basilar artery, which is formed by the convergence of the right and left vertebral arteries. These are responsible for the arterial supply to the occipital lobe.
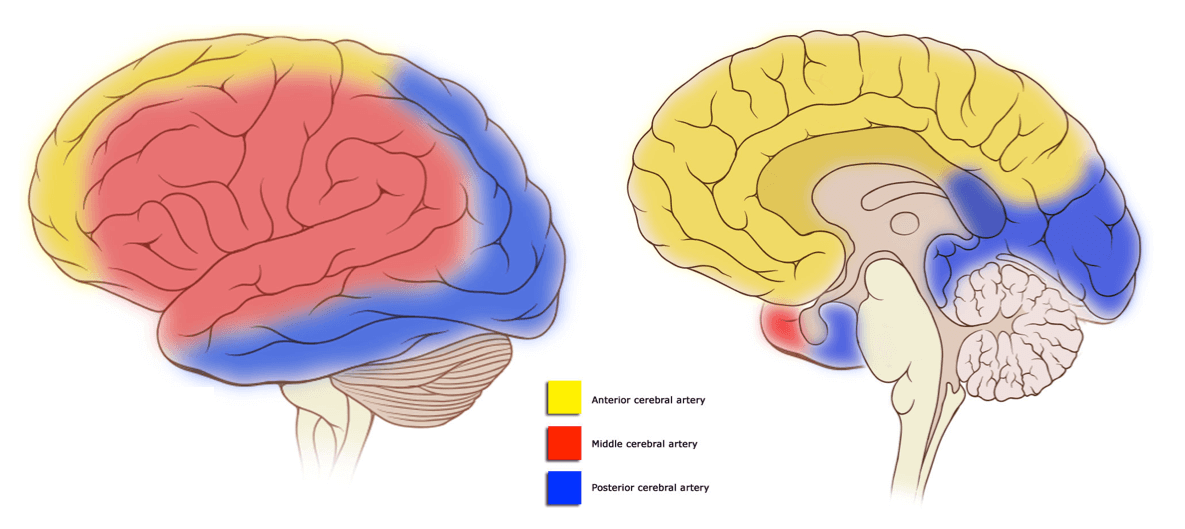
Cortical vascular territories, adapted from Wikipedia
Courtesy of OpenStax College CC BY-SA 2.5
Clinical features
The symptoms and signs of strokes vary depending upon which vascular territory is affected. The main symptoms of stroke according to territory are summarised in the table below:
| Blood vessel affected | Clinical features |
|---|---|
| Anterior cerebral artery | Contralateral motor weakness (leg/shoulder > arm/hand/face) Minimal contralateral sensory loss Dysarthria, aphasia Left limb apraxia Urinary incontinence Behavioural and personality changes |
| Middle cerebral artery | Contralateral hemiparesis (face/arm > leg) Contralateral hemisensory loss Expressive or receptive dysphasia (dominant hemisphere) Contralateral neglect (non-dominant hemisphere) |
| Posterior cerebral artery | Contralateral homonymous hemianopia Quadrantic visual field defects Contralateral thalamic syndrome (PCA supplies thalamus) |
Rapid recognition of symptoms and diagnosis
NICE recommend that in people with sudden onset of neurological symptoms a validated tool, such as FAST (Face Arm Speech Test), should be used outside the hospital to screen for a diagnosis of stroke or TIA.
The FAST acronym stands for:
- Facial drooping – a section of the face, usually only one side, is drooping and hard to move, e.g. a crooked smile
- Arm weakness, e.g. the inability to raise an arm fully or grip weakness
- Speech difficulty – an inability or difficulty in producing or understanding speech
- Time – if any of the above symptoms or signs are present, time is of the essence, and emergency services should be contacted immediately.

Any patient with an acute stroke should be sent immediately to an appropriate A&E department. A large number of trials have now confirmed the benefits of thrombolysis within 3 hours of developing symptoms.
In people with sudden onset of neurological symptoms, hypoglycaemia should always be excluded as the cause of these symptoms.
People who are admitted to the Emergency Department with a suspected stroke (or TIA) should have the diagnosis established rapidly using a validated tool, such as ROSIER (Recognition of Stroke in the Emergency Room).
Specialist care for people with acute stroke
All patients with a suspected stroke should be admitted to a specialist stroke unit either having been assessed by the GP or from A&E. Stroke units are used commonly, and the recommendation is that all patients where possible should be treated within this specialist settling.
Brain imaging should be performed immediately in patients with an acute stroke if any of the following apply:
- Indications for thrombolysis or early anticoagulation treatment
- On anticoagulant treatment
- A known bleeding tendency
- A depressed level of consciousness (Glasgow Coma Score below 13)
- Unexplained progressive or fluctuating symptoms
- Papilloedema, neck stiffness or fever
- Severe headache at onset of stroke symptoms.
Initial management of patients with suspected and confirmed TIA
The NICE recommendations for the management of patients with suspected TIA are as follows:
- Offer aspirin (300 mg daily), unless contraindicated, to people who have had a suspected TIA, to be started immediately.
- Refer immediately people who have had a suspected TIA for specialist assessment and investigation, to be seen within 24 hours of onset of symptoms.
- Do not use scoring systems, such as ABCD2, to assess risk of subsequent stroke or to inform urgency of referral for people who have had a suspected or confirmed TIA.
- Offer secondary prevention, in addition to aspirin, as soon as possible after the diagnosis of TIA is confirmed.
Imaging for people who have had a suspected TIA or acute non-disabling stroke
The NICE recommendations for imaging for people who have had a suspected TIA or acute non-disabling stroke are as follows:
- Do not offer CT brain scanning to people with a suspected TIA unless there is clinical suspicion of an alternative diagnosis that CT could detect.
- After specialist assessment in the TIA clinic, consider MRI (including diffusion-weighted and blood-sensitive sequences) to determine the territory of ischaemia, or to detect haemorrhage or alternative pathologies. If MRI is done, perform it on the same day as the assessment.
- Carotid imaging – everyone with TIA who after specialist assessment is considered as a candidate for carotid endarterectomy should have urgent carotid imaging.
Brain imaging for the early assessment of people with suspected acute stroke
The NICE recommendations for imaging for the early assessment of people with suspected acute stroke are as follows:
Perform brain imaging immediately with a non-enhanced CT for people with suspected acute stroke if any of the following apply:
- Indications for thrombolysis or thrombectomy
- On anticoagulant treatment
- A known bleeding tendency
- A depressed level of consciousness (Glasgow Coma Score below 13)
- Unexplained progressive or fluctuating symptoms
- Papilloedema, neck stiffness or fever
- Severe headache at onset of stroke symptoms.
If thrombectomy might be indicated, perform imaging with CT contrast angiography following initial non-enhanced CT. Add CT perfusion imaging (or MR equivalent) if thrombectomy might be indicated beyond 6 hours of symptom onset.
Perform scanning as soon as possible and within 24 hours of symptom onset in everyone with suspected acute stroke without indications for immediate brain imaging.
Further reading:
NICE Guideline: Stroke and transient ischaemic attack in over 16s: diagnosis and initial management
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this article.