Thermal burns are a significant cause of morbidity and mortality, but following the Advanced Trauma Life Support (ATLS) basic principles of initial trauma resuscitation and initiating simple emergency measures can significantly minimise their effect. It is estimated that in the UK approximately 250,000 people present with thermal burns each year. Of these patients, around 300 will go on to die as a result of the burn or subsequent complications.
The majority of these burns are minor and heal without any problems, but the cosmetic outcome is highly dependent upon appropriate burns care being administered in a timely fashion. The management during the first few days following the burn are of particular importance. Most simple thermal burns can be managed in primary care, but major and complex burns require specialist input, and a skilled multidisciplinary approach to ensure the best outcome.
Risk factors
The highest rates of thermal burns are seen in children under the age of 5 and the elderly over the age of 75. The kitchen is the most common site for thermal injures to occur with approximately 50% of burns and scalds occurring there. Toddlers are at particularly high risk of suffering burns in the kitchen from pulling hot beverages over themselves or from touching hot ovens or hobs.
The effects of heat on tissues
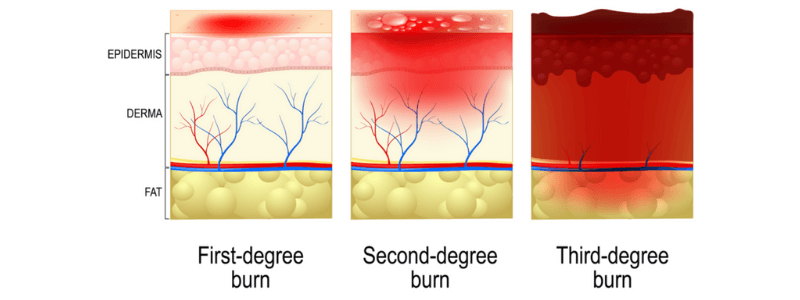
As temperature rises, proteins start to denature, and cellular function is compromised. Once a temperature of 40ºC is passed, cellular repair mechanisms fail, and cell death occurs. Temperatures above 60ºC cause tissue necrosis and thrombosis within blood vessels. Thermal injuries result in both local and systemic responses.
Local responses to thermal burns
The local response to a thermal burn is described in terms of the three zones of a burn. These burn zones were first described Mr. Douglas Jackson in 1947, and it is referred to as Jackson’s burn model:
Zone of coagulation: This occurs at the point of maximal damage and results from the direct thermal burn at the time of exposure. In this zone, there is irreversible tissue loss due to coagulation of the constituent proteins.
Zone of stasis: This zone surrounds the borders of the zone of coagulation. It is characterised by decreased tissue perfusion due to an inflammatory response and vascular reactivity that reduces blood flow in the area for around 24-48 hours after the thermal burn occurs. Burns resuscitation can help to increase tissue perfusion and prevent this damage from becoming irreversible. Prolonged hypotension and oedema can result in this zone becoming an area of complete tissue loss.
Zone of hyperaemia: This is the outermost area of the burn injury, and it is characterised by vasodilatation and increased blood flow that results in increased tissue perfusion. The tissue in this zone invariably recovers unless there is an additional insult, such as sepsis or prolonged hypotension.
Systemic responses to thermal burns
Thermal burns can also trigger an intense systemic inflammatory response as a result of the release of inflammatory mediators, such as cytokines, at the site of the injury. Any burn exceeding 30% of total body surface area (TBSA), tends to result in a profound systemic effect. The effects on each system are as follows:
Cardiovascular changes: Significant thermal burns result in an increase in capillary permeability that causes fluid and proteins to move from the intravascular space into the interstitial space. In response to this there is peripheral and splanchnic vasoconstriction and also reduced myocardial contractility, possibly due to the release of tumour necrosis factor α. In extensive burns, this results in significant oedema, hypovolaemia and end-organ hypoperfusion.
Respiratory changes: The release of inflammatory mediators can result in bronchoconstriction, and in extensive burns, adult respiratory distress syndrome and respiratory arrest can occur. There may also be an accompanying inhalation injury, resulting in airway damage and carbon monoxide poisoning.
Immunological changes: Significant burns result in down-regulation of the immune response. In the most severe cases, this immunosuppressed state can result in overwhelming sepsis.
Metabolic changes: Severe burns can cause significant metabolic derangement, and basal metabolic rate can increase as much as threefold. Nutritional support is of great importance and can be particularly challenging for burned patients. Early and aggressive enteral feeding is necessary to decrease catabolism and maintain gut integrity.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcemexamprep.net for this article.