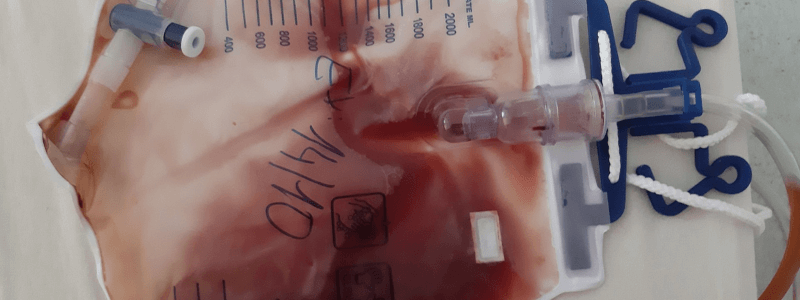
A 67-year-old man presents with painless haematuria that has persisted for several weeks. He denies any associated symptoms such as dysuria, fever, or flank pain. He reports a mild increase in urinary frequency but no urgency or nocturia. He has a past medical history of mild benign prostatic hyperplasia (BPH) and is otherwise in good health. He denies recent trauma or strenuous physical activity. His initial intravenous urogram (IVU) shows no abnormalities in the renal structure or urinary tract. Physical examination reveals a mildly enlarged prostate, consistent with age-related changes, but no tenderness or palpable masses.
Show Answer
The most likely diagnosis in this case is bladder cancer, given the patient’s age, painless haematuria, and lack of other specific symptoms or abnormalities on IVU. Bladder cancer is one of the most common causes of painless haematuria, particularly in older adults.
The risk factors for bladder cancer include:
- Advancing age (most cases occur in individuals over 60 years old)
- Male gender
- Smoking history (the strongest risk factor)
- Occupational exposures to certain chemicals (e.g., aniline dyes, rubber, leather)
- Chronic bladder inflammation or infections
Show Answer
The following investigations are recommended to confirm the diagnosis:
- Cystoscopy: This is the key investigation to directly visualise the bladder and check for any tumours or abnormalities.
- Urine cytology: This test can detect cancerous cells shed into the urine.
- CT urogram or MRI: These can help evaluate the upper urinary tract (kidneys, ureters) and stage any tumour that might be detected.
Show Answer
The treatment of bladder cancer depends on the stage and grade of the tumour.
For non-muscle invasive bladder cancer (NMIBC), which is confined to the bladder lining, the primary treatment is:
- Transurethral resection of the bladder tumour (TURBT): This removes the tumour tissue.
- Intravesical therapy: Following TURBT, medications such as Bacillus Calmette-Guerin (BCG) or mitomycin may be instilled into the bladder to reduce the risk of recurrence.
For muscle-invasive bladder cancer (MIBC), treatment may include:
- Radical cystectomy (removal of the bladder) with urinary diversion.
- Chemotherapy or radiation therapy, depending on the case.
Close follow-up with repeat cystoscopy is critical for detecting any recurrence, as bladder cancer has a high rate of recurrence.