Acute epiglottitis is inflammation of the epiglottis. When there is involvement of the soft tissues surrounding the epiglottis, then it is referred to as acute supraglottitis. It can result in life-threatening airway obstruction and death if rapid treatment is not instituted. The most common age at presentation is between the ages of 3 and 5; it can, however, affect any age with adults presenting in their 40s and 50s.
Historically the most common causative organism was Haemophilus influenza type B, but since the introduction of Haemophilus influenza type B (Hib) vaccination, it has become rare in childhood and the majority of cases are now caused by Streptococcus spp. Other potential causative organisms include Staphylococcus aureus, Pseudomonas spp., Moraxella catarrhalis, Mycobacterium tuberculosis and the herpes simplex virus. Candida spp. and Aspergillus spp. Infection can occur in immunocompromised patients.
The typical clinical features of acute epiglottitis include:
- Fever
- Sore throat
- Odynophagia
- Dysphagia
- Inability to swallow secretions (drooling in children)
- Muffled voice – ‘hot potato’ voice
- Stridor
- Respiratory distress
- Tachycardia
- Anterior neck tenderness over the hyoid bone
- Ear pain
- Cervical lymphadenopathy
Patients may also adopt the tripod position, leaning forward with their arms extended and hands resting on their knees or a surface. This posture helps to shift inflamed supraglottic structures forward, temporarily relieving airway obstruction.
Fibre-optic laryngoscopy remains the gold standard for diagnosing acute epiglottitis. However, it should only be performed by an experienced anaesthetist in a fully equipped setting, where immediate airway intervention — such as intubation or tracheostomy — can be safely carried out if obstruction occurs.
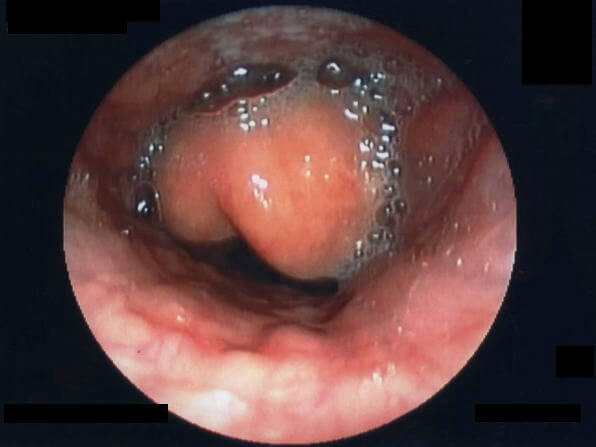
Inflamed epiglottitis seen on fibre-optic laryngoscopy Wikipedia
Courtesy of Wikimedia Commons CC BY-SA 3.0
Other useful investigations, once the patient has been stabilised include:
- Lateral neck X-ray (thumbprint sign)
- Throat swabs
- Blood cultures
- CT neck (for suspected abscess formation)
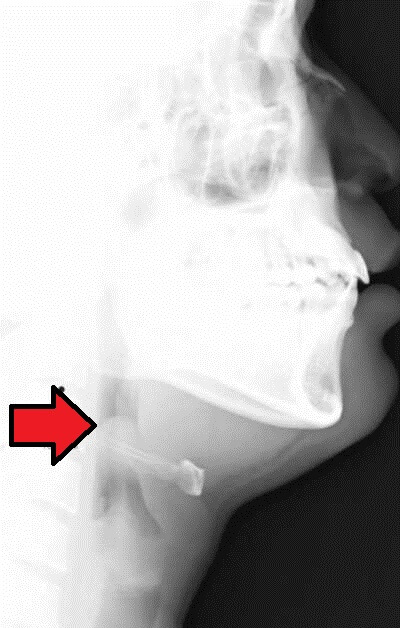
Thumbprint sign’ on lateral neck X-ray
Acute epiglottitis is a medical emergency. Particularly with a paediatric presentation, it is essential not to panic or distress the patient. Do not attempt to examine the throat and visualise the epiglottitis using a tongue depressor as this is likely to provoke spasm and provoke airway obstruction. Keep the patient as calm as possible.
The first step should be to call a senior anaesthetist immediately. A senior paediatrician and ENT surgeon should also be called. Nebulised adrenaline can be used as an interim measure if airway compromise is imminent and an experienced anaesthetist is not present.
Unless there is accompanying circulatory collapse, intravenous access should be left until the airway is secured.
Antibiotic treatment for confirmed diagnosis once the airway has been secured is usually with intravenous ceftriaxone (2 g OD). Levofloxacin plus teicoplanin is an alternative for penicillin-allergic patients. Local policy and guidelines should be followed.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.plabprep.co.uk for this article.







Good article particularly useful emergency information
Good information
Good information