Cyanotic congenital heart disease (CHD) typically involves right-to-left or mixed circulations, resulting in systemic desaturation. In adult imaging, most cases you encounter will be in patients with repaired or palliated anatomy. Others may present with long-standing complications or late diagnoses.
This section covers five high-yield lesions relevant to both exams and clinical reporting:
- Tetralogy of Fallot
- Transposition of the Great Arteries
- Eisenmenger physiology
- Total Anomalous Pulmonary Venous Return
- Truncus Arteriosus
Tetralogy of Fallot (ToF)
Tetralogy of Fallot is one of the most frequently repaired cyanotic heart lesions seen in adult imaging. It consists of four key features:
- Ventricular septal defect (VSD)
- Right ventricular outflow tract (RVOT) obstruction
- Overriding aorta
- Right ventricular hypertrophy
Before surgical repair, chest radiographs may show features classically described as a ‘boot-shaped’ cardiac silhouette, with an upturned apex and a concave pulmonary segment. Pulmonary vascular markings may be reduced. These signs are more commonly seen in unrepaired cases or historical examples.
Post-repair, imaging focuses on long-term complications:
- MRI is the preferred modality for assessing right ventricular volumes, pulmonary regurgitation, and residual RVOT obstruction.
- CT may be useful for evaluating surgical conduits or prosthetic material, especially if MRI is contraindicated.
Reporting points:
- Assess right ventricular size and function
- Document pulmonary valve competence and regurgitation
- Look for residual VSD, aneurysm, or conduit narrowing
- Comment on aortic dimensions, as dilatation is a known late finding
Transposition of the Great Arteries (TGA)
Transposition involves abnormal ventriculo-arterial connections.
Two major types:
- Dextro-TGA (d-TGA): Aorta arises from the right ventricle, pulmonary artery from the left; requires neonatal intervention for survival
- Levo-TGA (l-TGA): Also called congenitally corrected TGA; involves AV and VA discordance with the morphologic right ventricle supporting systemic circulation
Post-operative anatomy in d-TGA depends on surgical approach:
- Arterial switch (Jatene procedure): Aorta and pulmonary artery positions corrected
- Atrial switch (Mustard/Senning): Venous return redirected via intra-atrial baffles, with morphologic RV remaining systemic
Imaging considerations:
- MRI is essential for long-term follow-up in both types. In atrial switch patients, systemic right ventricular failure and tricuspid regurgitation are key concerns.
- CT is useful for coronary artery assessment post-arterial switch and for baffle evaluation when MRI is suboptimal.
Reporting points:
- Define the surgical repair
- Assess systemic ventricular function
- Look for baffle stenosis or leaks in atrial switch
- Evaluate the neo-aortic root (original pulmonary root) and neo-pulmonary artery dimension
Eisenmenger Physiology
This represents the natural progression of large, uncorrected left-to-right shunts such as VSD, ASD, or PDA. Over time, pulmonary vascular resistance increases, reversing the shunt and causing systemic desaturation.
Imaging findings:
- Chest radiograph: Enlarged central pulmonary arteries and peripheral vascular pruning. The diameter difference between the central and the peripheral pulmonary arteries can be extreme; enormous pulmonary arteries may be the most striking imaging finding in advanced cases.
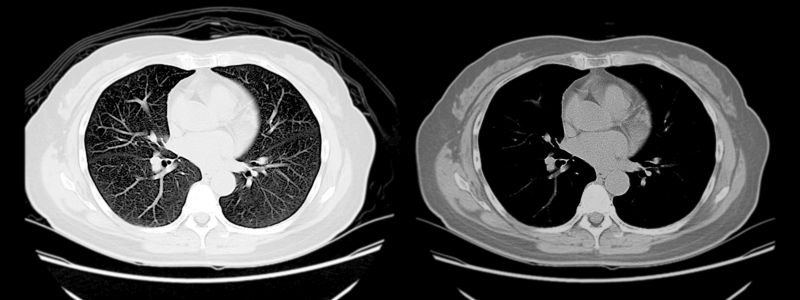
- CT: Markedly dilated pulmonary arteries, right ventricular hypertrophy, and possible in situ thrombosis
- MRI: Shows interventricular septal bowing during systole, indicating pressure overload, along with right heart dysfunction and reversed or bidirectional shunt flow through the original defect
Avoid relying on numeric thresholds. Instead, describe the relative size of the main pulmonary artery and its impact on adjacent structures.
Reporting points:
- Describe right heart size and septal position
- Look for mural thrombus in dilated arteries
- Identify the original shunt lesion, if visible
- Confirm reversal of flow where applicable
Total Anomalous Pulmonary Venous Return (TAPVR)
In TAPVR, all pulmonary veins drain into the systemic venous circulation instead of the left atrium. An interatrial communication is required for survival.
Types:
- Supracardiac: Pulmonary veins drain to the left innominate vein via a vertical vein
- Cardiac: Drainage to the right atrium or coronary sinus
- Infracardiac: Through the portal or hepatic system; often obstructed
- Mixed: Features of more than one subtype
Imaging findings:
- Chest radiograph: The supracardiac type may show the ‘snowman’ sign (seen best on frontal view)
- CT/MRI: Clearly delineates the anomalous venous pathways and any associated narrowing or obstruction
- Echo: May be diagnostic in infants; often limited in adults due to suboptimal windows and complex post-surgical anatomy
Reporting points:
- Identify the anomalous venous connection(s)
- Confirm the presence and size of interatrial communication
- Assess for post-surgical narrowing or pulmonary venous obstruction
Truncus Arteriosus
In truncus arteriosus, a single arterial trunk arises from the heart and gives rise to the coronary, systemic, and pulmonary circulations. This always coexists with a large VSD.
Imaging findings:
- CT/MRI: Shows a single overriding vessel, with pulmonary arteries branching directly from it. MRI also provides functional data.
- Echo: May detect truncal valve regurgitation or stenosis
Post-repair imaging:
- Surgical management involves separating pulmonary and systemic circulations using a conduit.
- MRI is used to assess truncal valve function, conduit patency, and ventricular performance.
Reporting points:
- Comment on conduit integrity and valve competence
- Assess for regurgitation or stenosis
- Measure ventricular volumes and function
Summary Points
Cyanotic congenital lesions are rarely seen in their native form in adult practice. Most patients have undergone surgical intervention and are being monitored for long-term complications. As the reporting radiologist, your responsibilities include:
- Describing the current anatomy and any surgical modifications
- Assessing systemic ventricular function and flow patterns
- Identifying post-operative issues such as regurgitation, conduit stenosis, or pulmonary hypertension
- Avoid vague descriptions – be specific about anatomical findings and surgical modifications
Recognising these repaired lesions and their complications is a core skill – especially for MRI and CT interpretation in adult congenital patients. These cases are also tested in the FRCR, where clear, structured reporting can set your answers apart.
Header image used on licence from Shutterstock.
Thank you to the joint editorial team of FRCR Exam Prep for this article.