Septic arthritis is a purulent invasion of a joint by an infectious agent, usually caused by bacteria, but it can also be caused by viruses or fungi. It is usually monoarticular and most commonly affects the knee or hip. If left untreated, it can result in potential joint destruction and sepsis.
Pathophysiology
Septic arthritis occurs when microorganisms invade the synovial joint space, leading to an acute inflammatory response with the recruitment of neutrophils and the production of proteolytic enzymes that damage cartilage and joint structures.
The routes of infection are:
- Haematogenous spread: Most common route, typically secondary to bacteraemia.
- Direct spread: This can be from penetrating trauma, surgery or via neighbouring infections (e.g. osteomyelitis).
- Contiguous spread: From adjacent infected tissues.
Causative organisms include:
- Staphylococcus aureus (most common overall cause in both adults and children)
- Streptococcus spp.
- Haemophilus influenzae (previously common in children, but now rare due to vaccination).
- Neisseria gonorrhoea (typically sexually active young adults, macules or vesicles frequently seen on the trunk)
- Escherichia coli (seen in IVDUs, the elderly and seriously ill
- Kingella kingae (seen in young children between 6 to 36 months).
- Mycobacterium tuberculosis (causes chronic infection – tuberculous arthritis).
- Fungi, e.g. Histoplasma spp. (rare, seen in immunocompromised patients).
Risk factors
Risk factors include:
- Age: Extremes of age (children and elderly).
- Joint disease: Pre-existing arthritis (e.g. osteoarthritis, rheumatoid arthritis and gout).
- Immunosuppression: Diabetes, HIV, malignancy and steroid use.
- IV drug use: Increased risk of Gram-negative and polymicrobial infections.
- Trauma/surgery: Penetrating injuries or recent joint surgery can cause direct inoculation of bacteria into the joint.
- Sexually active young adults: Higher risk for Neisseria gonorrhoea infections.
Clinical features
The knee is the most affected joint. Other commonly affected joints include the hip, shoulder, ankle and wrist.
Typical clinical features of septic arthritis include:
- Sudden-onset severe pain in the affected joint.
- Visible swelling and joint effusion.
- Overlying skin may be red and warm.
- Pain exacerbated by active/passive movement.
- Inability to move joint common.
- Fever, rigors, and tachycardias.
- Sepsis in severe cases.
Presentation in young children, particularly when the hip is involved can be subtle, and often the only clinical features are refusal to weight bear and irritability.
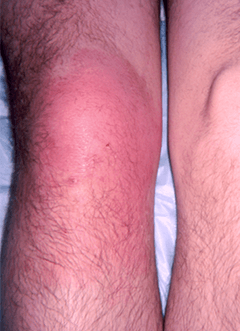
Septic arthritis of the right knee
Complications
Potential complications include:
- Joint destruction: Rapid cartilage loss and progression to osteoarthritis.
- Sepsis: Disseminated infection leading to multi-organ failure.
- Osteomyelitis: Spread of infection to the bone.
- Ankylosis: Fibrous or bony fusion causing joint stiffness.
Investigations
Blood tests:
- FBC (leucocytosis).
- CRP/ESR (raised markers of inflammation).
- Blood cultures (to identify bacteraemia – positive in ~50% of cases).
Joint aspiration:
- Joint aspiration is the gold-standard diagnostic investigation for septic arthritis.
- Appearance: turbid or purulent synovial fluid.
- White cell count: WCC: >50,000 cells/mm³ (neutrophil predominance).
- Gram-stain and culture: Identifies causative organism.
- Crystal analysis: To exclude gout or pseudogout.
Imaging:
- Plain X-ray: Often normal early in the presentation. May show soft tissue swelling and joint space widening in late stages.
- Ultrasound: Detects effusion, especially in deep joints, such as the hip.
- MRI/CT: Can be considered as part of the evaluation of suspected infections of certain joints (e.g. sternoclavicular or sacroiliac joints) or to assess complications.
- Radionuclide scans: Can be helpful for diagnosing infections in isolated or deep joints (e.g. sacroiliac joints).
Management
Initial Emergency Department management:
- In patients with signs of sepsis, resuscitation and stabilisation are the immediate priority.
- The patient should be made comfortable and provided with suitable analgesia.
- The joint should ideally be aspirated before antibiotics are given. Aspirating the joint to dryness will also relieve pressure and ease discomfort.
- The patient should be referred to the on-call Orthopaedic team for inpatient management and potential surgical drainage.
Empirical IV antibiotics:
- Empirical antibiotics should be started immediately after joint aspiration and blood cultures have been sent to the laboratory.
- The choice of antibiotic can be adjusted once culture results are available.
- Antibiotics are typically needed for 4-6 weeks and potentially longer if complications arise.
- Local policies and guidelines should be followed, but typical choices of antibiotics are shown in the table below:
|
Scenario
|
Antibiotic choice |
|
First-line for native joint
|
IV flucloxacillin |
|
Penicillin allergy
|
IV clindamycin |
|
MRSA risk |
IV vancomycin
|
|
Gonococcal arthritis |
IV cefotaxime
|
|
Suspected Gram-negative infection or immunocompromised
|
IV cefotaxime ± gentamicin
|
|
Prosthetic joint |
IV Vvncomycin + rifampicin ± gentamicin
|
Surgical intervention:
- Indications for surgical joint drainage include a persistent or large effusion that is resistant to drainage by aspiration, hip involvement (nearly always requires surgery), adjacent soft tissue involvement, septicaemia or rapid joint destruction.
- Options include arthroscopic Lavage (most common) and open arthrotomy for large effusions or deep joints.
🔑 Key takeaways for MRCEM SBA
✅ Septic arthritis is a medical emergency – requires urgent diagnosis and treatment to prevent joint destruction and sepsis.
✅ Most commonly affects the knee, followed by hip, shoulder, ankle, and wrist.
✅ Pathophysiology: Microbial invasion → Neutrophilic inflammation → Cartilage destruction → Risk of sepsis & osteomyelitis.
✅ Common causative organisms:
- Staphylococcus aureus (most common in all ages).
- Neisseria gonorrhoea (sexually active young adults).
- Kingella kingae (young children).
- Gram-negative bacteria (elderly, IVDU, immunocompromised).
✅ Risk factors: Age extremes, joint disease (RA, OA, gout), immunosuppression, IVDU, trauma, surgery.
✅ Clinical features:
- Sudden-onset joint pain, swelling, erythema, warmth, effusion.
- Severe pain on passive & active movement.
- Fever, rigors, tachycardia, systemic signs of sepsis.
- Refusal to weight-bear (important in children with hip involvement).
✅ Key investigations:
- Joint aspiration (gold standard) → Turbid/purulent fluid, WCC >50,000 cells/mm³, neutrophil predominance.
- Gram stain & culture → Identifies pathogen.
- Blood cultures (~50% positive), CRP, ESR, FBC (leucocytosis).
- Imaging: X-ray (late changes), ultrasound (effusion), MRI/CT (deep joints, complications).
✅ Management:
- Urgent orthopaedic referral + joint aspiration for diagnosis & symptom relief.
- Empirical IV antibiotics immediately after aspiration – flucloxacillin (1st line), vancomycin for MRSA risk.
- Surgical drainage if required – Arthroscopic lavage or open arthrotomy for deep/large effusions.
- Total antibiotic duration: 4–6 weeks.
✅ Complications: Joint destruction, osteomyelitis, ankylosis, sepsis, multi-organ failure.
Thank you to the joint editorial team of www.mrcemexamprep.net for this ‘Exam Tips’ blog post.






VOILA!!!