A 24-year-old man presents complaining of recurrent episodes of abdominal pain and passing dark brown urine first thing in the morning. On examination, he has raised, painful, red nodules on the skin covering his entire back. You organise a set of blood tests, which reveal the presence of a haemolytic anaemia, leukopenia and thrombocytopenia.
- What is the most likely diagnosis?
Show Answer
The most likely diagnosis in this case is paroxysmal nocturnal haemoglobinuria.
Paroxysmal nocturnal haemoglobinuria is a rare acquired genetic disorder that can affect all haematological cells. It is caused by a haematopoietic stem cell mutation defect of the PIGA gene on the X-chromosome. In PNH there is a marked deficiency or absence of the complement regulatory proteins CD55 and CD59.
This mutation results in increased sensitivity of the cell membranes to the action of the patient’s own complement, which damages red cells, white cells, platelets and stem cells. This in turn, results in intravascular haemolysis with haemoglobinuria, leukopenia and thrombocytopenia.
The three main features of the disease are:
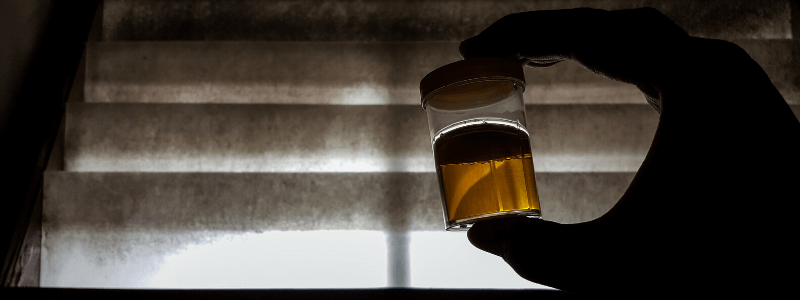
- Haemolytic anaemia. This is the most common presentation. Haemoglobinuria, particularly first thing in the morning or last thing at night, occurs and can be mistaken for heamaturia. The urine will be dark brown in colour.
- Thrombosis. This generally affects the veins and tends to affect t hepatic, abdominal, cerebral and subdermal veins. The mode of presentation depends upon which veins are involved (e.g. abdominal veins causing abdominal pain). Thrombosis of dermal veins can cause raised, painful, red nodules in the skin covering large areas (e.g. the back). Budd-Chiari syndrome can occur resulting in hepatomegaly and ascites.
- Deficient haematopoiesis. This can result in symptoms of anaemia-like shortness of breath and fatigue. In severe cases pancytopenia can occur.
- How can this diagnosis be confirmed?
Show Answer
The results of investigations can include the following:
- Urine dipstick for blood will be positive but microscopy will not show red blood cells, confirming that it is haemoglobinuria and not haematuria.
- Full blood count usually reveals normochromic, normocytic anaemia.
- Leukopenia and thrombocytopenia can also be present.
- Serum LDH is raised
- Leukocyte alkaline phosphatase may be reduced
- Negative Coomb’s test
- Bone marrow is variable (either hypoplasia or erythroid hyperplasia)
A definitive diagnosis can be made using flow cytometry to detect the complement regulatory proteins CD55 (DAF) and CD59 (MIRL). Absence or reduced expression of both CD55 and CD59 is diagnostic for PNH.
Show Answer
Treatment of PNH is largely symptomatic and includes the following:
- Blood transfusion may be required but leukocyte depletion is necessary to reduce antibody formation aggravating haemolysis.
- Meningococcal vaccination is essential because of the associated risk of meningococcal infection
- Eculizumab a humanised monoclonal antibody that binds and prevents activation of complement C5 and the subsequent formation of the cytolytic membrane attack complex of complement. Administered by infusion under expert guidance.
- Anticoagulation to reduce the risk of thrombosis
- Prednisolone during periods of haemolysis (effective in approximately 70% of cases)
- Bone marrow transplantation may be required in severe cases.
Prognosis varies greatly depending upon the severity and complications developed. Thromboembolism is the most common cause of death (approximately 40-65% of deaths in PNH).
Header used on licence from Shutterstock





good question
Really a refreshing question
Thank u very much Sir
thank you verry much sir.