Lung volumes, which are also known as respiratory volumes, refer to the various volumes of gas in the lungs at any given time during the respiratory cycle. Lung capacities are derived from a summation of different lung volumes. It is important to have an understanding of lung volumes and capacities and the definitions of these in adults.
Definitions and typical lung volumes
The tidal volume (TV) is the volume of air drawn in and out of the lungs during normal breathing. The usual volume in a healthy male is 0.5 L.
The vital capacity (VC) is the maximum volume of air that can be breathed out following a maximal inspiration. The usual volume in a healthy male is 4.5 L.
The residual volume (RV) is the volume of air in the lungs after a maximum expiration. The usual volume in a healthy male is 1.0 L.
The inspiratory reserve volume (IRV) is the maximum volume of air that can be breathed in during maximal inspiration. The usual volume in a healthy male is 3.0 L.
The expiratory reserve volume (ERV) is the maximum volume of air that can be breathed out during maximal expiration. The usual volume in a healthy male is 1.0 L.
Total lung capacity (TLC) is the volume of air in the lungs at the end of a maximal inspiration. TLC = RV+VC. The usual volume in a healthy male is 5.5 L.
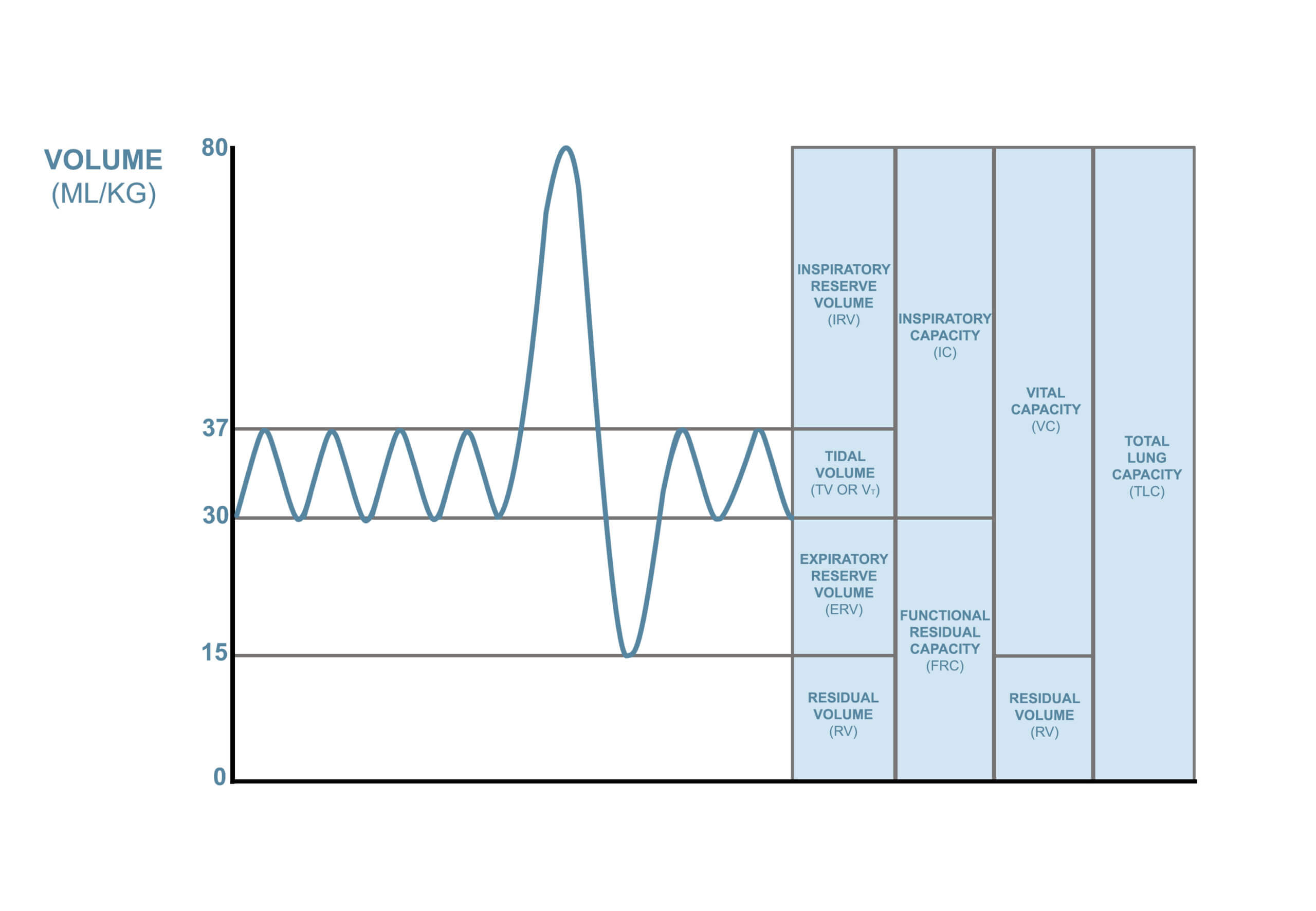
Image © Medical Exam Prep
The functional residual capacity
The functional residual capacity (FRC) is the volume of air present in the lungs at the end of a normal expiration. The usual volume in a healthy male is 2.0 L. At FRC, the opposing elastic recoil forces of the lungs and chest wall are in equilibrium, and there is no exertion by the diaphragm or other respiratory muscles.
The FRC is the sum of the expiratory reserve volume (ERV) and the residual volume (RV):
FRC = ERV + RV
The FRC cannot be estimated by spirometry as it includes the residual volume. In order to measure the RV precisely, one of the following methods is needed:
- Nitrogen washout (Fowler’s method)
- Helium dilution technique
- Body plethysmography
The FRC is increased by the following:
- Marked airway obstruction (e.g. severe asthma and COPD)
- Loss of elastic recoil (e.g. advanced age and emphysema)
The FRC is reduced by the following:
- Abnormally stiff, non-compliant lungs (e.g. restrictive lung disorders such as pulmonary fibrosis)
- Bilateral paralysis of the diaphragm
- Lying in the supine position
- Induction of anaesthesia (FRC falls by 15-20%)
Pre-oxygenation and the FRC
Pre-oxygenation is the administration of oxygen to a patient prior to intubation. It helps to extend the ‘safe apnoea time’. The ‘safe apnoea time’ is defined as the duration of time following cessation of breathing/ventilation that elapses until arterial desaturation occurs (SaO2 reaches < 90%)
The primary mechanism by which pre-oxygenation works is by ‘denitrogenation’ of the lungs, however maximal pre-oxygenation is achieved when the alveolar, arterial, venous and tissue compartments are all filled with oxygen. Denitrogenation is achieved using oxygen to wash out the nitrogen contained in the lungs after breathing room air, resulting in a larger alveolar oxygen reservoir.
The FRC is the most important store of oxygen in the body. The greater the FRC, the longer apnoea can be tolerated before critical hypoxia develops. Patients with reduced FRC (e.g. lung disease, kyphoscoliosis, pregnancy, and obesity) reach critical hypoxia more rapidly. The aim of pre-oxygenation is to replace nitrogen in the FRC with oxygen.
Dead space
Dead space is defined as the volume of inhaled air that does not take part in gas exchange.
The dead space can be further classified into:
- Anatomical dead space: The portion of the airways that conducts gas to the alveoli. No gas exchange is possible in these spaces
- Alveolar dead space: The sum of the volumes of those alveoli that have little or no blood flowing through their adjacent capillaries, i.e. the alveoli that are ventilated but not perfused. This is negligible in healthy people but can increase considerably in individuals with lung disease that causes ventilation-perfusion mismatch.
- Physiological dead space: the sum of the anatomical and alveolar dead spaces. The physiological dead space can account for up to 30% of the tidal volume.
The alveolar dead space is negligible in healthy adults but can increase dramatically in the presence of lung disease (e.g. pulmonary embolus, pneumonia) due to ventilation-perfusion mismatch.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcemexamprep.net for this ‘Exam Tips’ blog post.






