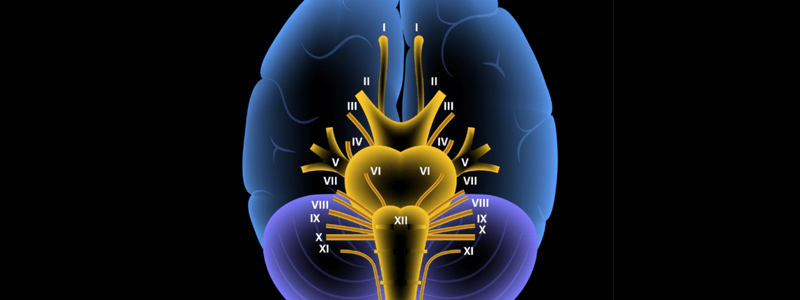
There are twelve paired cranial nerves in total, and they all arise directly from the brain, in contrast to the spinal nerves, which arise from segments of the spinal cord.
The cranial nerves are accordingly numbered by the location within the brainstem (superior to inferior then medial to lateral) and the order of their exit from the cranium (anterior to posterior).
The origin of the cranial nerves
The first two cranial nerves, the olfactory nerve and the optic nerve, arise from the cerebrum, whereas the remaining ten cranial nerves arise from the brainstem. They either arise from a specific part of the brainstem (midbrain, pons, or medulla) or from a junction between the two parts.
Cranial nerves III-XII arise from the following locations within the brainstem:
| Location arisen from | Cranial nerve |
|---|---|
| Midbrain | Trochlear nerve (CN IV) |
| Midbrain-pontine junction | Oculomotor nerve (CN III) |
| Pons | Trigeminal nerve (CN V) |
| Pontine-medulla junction | Abducens nerve (CN VI) Facial nerve (VII) Vestibulocochlear nerve (CN VIII) |
| Medulla oblongata (posterior to the olive) | Glossopharyngeal nerve (CN IX) Vagus nerve (CN X) Accessory nerve (CN XI) |
| Medulla oblongata (anterior to the olive) | Hypoglossal nerve (CN XII) |
Location of exit of the cranial nerves
The cranial nerves exit the skull at the following anatomical locations:
| Anatomical location | Cranial nerve |
| Cribriform plate | Olfactory nerve (CN I) |
| Optic foramen | Optic nerve (CN II) |
| Superior orbital fissure | Oculomotor nerve (CN III) Trochlear nerve (CN IV) Trigeminal nerve (CN V1 – Ophthalmic nerve) Abducens nerve (CN VI) |
| Foramen rotundum | Trigeminal nerve (CN V2 – Maxillary nerve) |
| Foramen ovale | Trigeminal nerve (CN V3 – Mandibular nerve) |
| Internal auditory canal | Facial nerve (CN VII) Vestibulocochlear nerve (CN VIII) |
| Jugular foramen | Glossopharyngeal nerve (CN IX) Vagus nerve (CN X) Accessory nerve (CN XI) |
| Hypoglossal canal | Hypoglossal nerve (CN XII) |
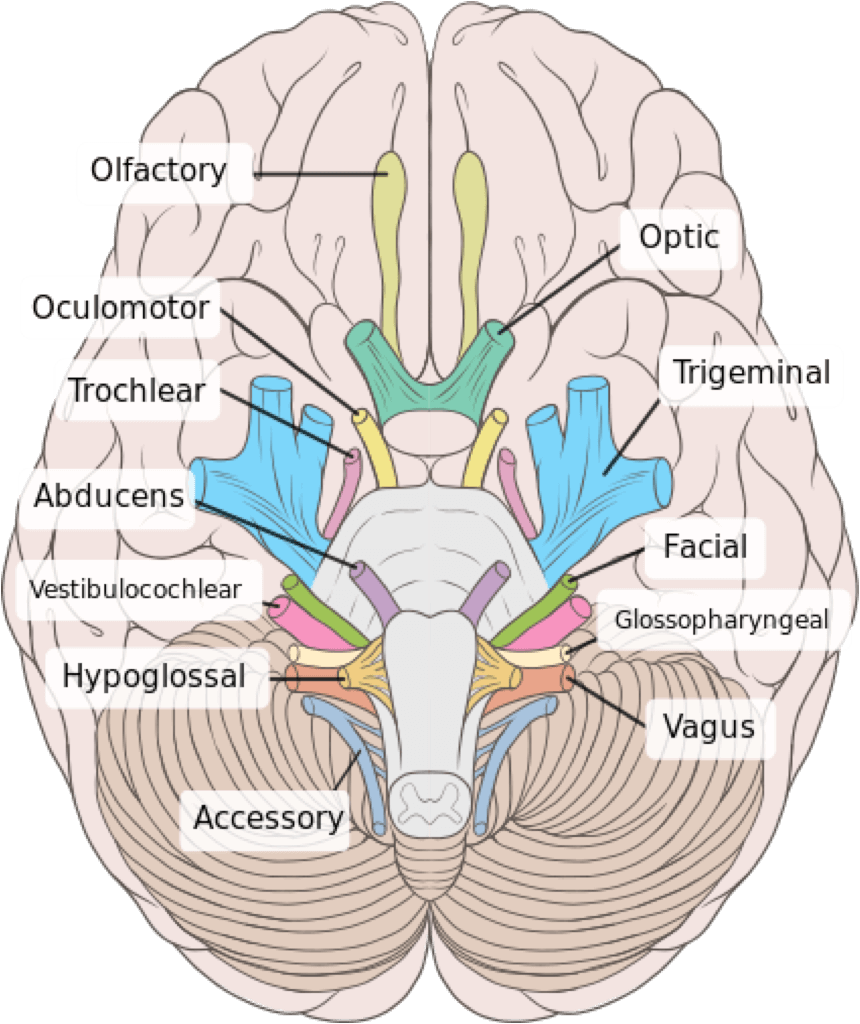
Image sourced from Wikipedia
Courtesy of Patrick J. Lynch CC BY-SA 2.5
Function of the cranial nerves
The function of the cranial nerves is summarised in the table below:
| Cranial nerve | Function |
|---|---|
| Olfactory nerve (CN I) | Smell |
| Optic nerve (CN II) | Vision |
| Oculomotor nerve (CN III) | Raises eyelid Eye movements Pupil constriction Lens accommodation |
| Trochlear nerve (CN IV) | Eye abduction and intortion Downward gaze |
| Trigeminal nerve (CN V1 – Ophthalmic nerve) | Scalp, forehead and corneal sensation |
| Trigeminal nerve (CN V2 – Maxillary nerve) | Palate, nasal cavity, and maxillary sensation |
| Trigeminal nerve (CN V3 – Mandibular nerve) | Mandibular sensation Anterior 2/3 of tongue sensation Mastication |
| Abducens nerve (CN VI) | Eye abduction |
| Facial nerve (CN VII) | Facial sensation Control of amplitude of hearing Posterior 1/3 of tongue sensation |
| Vestibulocochlear nerve (CN VIII) | Hearing Balance |
| Glossopharyngeal nerve (CN IX) | Elevation of pharynx Salivation Posterior 1/3 of tongue sensation |
| Vagus nerve (CN X) | Swallowing Phonation Laryngeal sensation |
| Accessory nerve (CN XI) | Head rotation to opposite side Elevation and rotation of scapula |
| Hypoglossal nerve (CN XII) | Tongue movement |
Lesions of the cranial nerves
Lesions of the cranial nerves are outlined below:
Olfactory nerve (I)
A lesion of the olfactory nerve results in reduced smell and taste (except to ammonia which is carried in the trigeminal nerve as it stimulates the pain fibres).
Optic nerve (II)
Optic nerve lesions are complex, and the clinical manifestation depends on where they occur in the visual pathway. They cause a variety of defects, including hemianopias, quadrantanopias, sectoral defects and scotomas.
Oculomotor nerve (III)
Oculomotor nerve lesions usually result in a fixed, dilated pupil that does not accommodate. An unopposed lateral rectus results in the eye appearing ‘down and out’.
Trochlear nerve (IV)
The trochlear nerve supplies the superior oblique muscle, which abducts, depresses and internally rotates the eye. Lesions cause vertical diplopia, and patients commonly tilt or lean their heads to allow better alignment of the eyes to compensate.
Trigeminal nerve (V)
The trigeminal nerve forms three trunks, the ophthalmic, maxillary and mandibular divisions. Lesions cause reduced sensation over whichever branch is involved. The ophthalmic division is also responsible for the corneal reflex. The mandibular division also supplies motor fibres to the masseter, temporalis and pterygoids. Lesions of this division, therefore, also cause weakness of jaw clenching and side-to-side movement. If the lesion is a lower motor one, the jaw deviates to the side of the lesion.
Abducens nerve (VI)
The abducens nerve supplies the lateral rectus muscle, which is responsible for abducting the eye. A lesion here results in the patient being unable to look laterally. The unopposed action of the medial rectus results in the eye being deviated medially. This commonly causes diplopia.
Facial nerve (VII)
Facial nerve lesions cause weakness of the facial muscles. If the lesion is a lower motor neuron one (as in Bell’s palsy), the forehead is involved, but if it is an upper motor neuron lesion, the forehead is spared because of bilateral innveration.
Vestibulocochlear nerve (VIII)
Vestibulocochlear nerve lesions result in unilateral sensorineural deafness and tinnitus.
Glossopharyngeal nerve (IX)
The glossopharyngeal nerve receives sensory fibres from the tonsils, pharynx, middle ear and posterior 1/3 of the tongue. It also receives visceral sensory fibres from the carotid sinus and carotid bodies. Its only motor fibre supplies the stylopharyngeus muscle. Bilateral lesions here cause pseudobulbar palsy.
Vagus nerve (X)
The vagus nerve supplies motor fibres to the palate and vocal cords and sensory fibres to the external acoustic meatus. Lesions can cause asymmetrical movement of the palate, nasal regurgitation of food and a nasal quality to the voice.
Accessory nerve (XI)
The accessory nerve gives motor supply to the sternocleidomastoid and trapezius muscles. A lesion here causes weakness of these muscles.
Hypoglossal nerve (XII)
The hypoglossal nerve supplies motor fibres to the tongue and infrahyoid muscles. A lower motor lesion here causes fasciculation and wasting of the ipsilateral muscles of the tongue, and when the tongue is stuck out, it deviates to the side of the lesion. With an upper motor lesion, the tongue deviates away from the side of the lesion.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcemexamprep.net for this ‘Exam Tips’ blog post.





Well Stacked !
Thank you.