I’m sure by now most of you are asking what on earth the oxygenator is. To be honest, I asked it too. I had to think of a way to get you thinking about an often neglected area of patient assessment… neglect of which can be catastrophic. As I started thinking about it, I realized this area is huge, complex, anatomically variable, angulated and extends much further than we realize to a circulatory fluid begging for nutrients. Confused?? Yeah, me too, but let’s begin.
The oxygenator is actually the AIRWAY. I hear you all saying that’s just silly. The airway is easy-peasy – mouth to larynx – what’s the big deal? In short… no breath, no life. No oxygen, no life. I don’t care how clever you are, how incredible your recall for the differentials on the ward round, if you can’t oxygenate your patient, you are useless to the sickest of sick.
How many of you routinely assess the oxygenator? Perhaps anaesthetists, intensivists, and ED physicians do, but the rest? I doubt it’s done. It usually is considered when there is distress, which is when it is late in the game and inexorably leading to a deoxygenation. So if it is such a serious issue, why is it neglected? I personally think it is because it is not seen as a portal for oxygen delivery. It is viewed as ANATOMY. It’s seen as the anatomical preserve of the ENT surgeon or the anaesthetist. It is excitedly “intubated” by eager medical students and interns to later brag about their respective skills. But this is not it. The emphasis is poorly placed. Let’s start again….
Oxygen is our number 1 ‘electrolyte’, it is fundamental to generating adequate ATP, via an electron transport chain. This occurs at a cellular level, deep within the mitochondria. But how did it get there? A quick journey will elucidate its travels, starting from the mitochondria and working back…
Mitochondria → cytoplasm → RBC/Hb + blood → arteries → aorta → left ventricle → left atrium → pulmonary veins → alveolar capillaries → alveoli → tracheobronchial tree → larynx → pharynx → nose/mouth → atmosphere
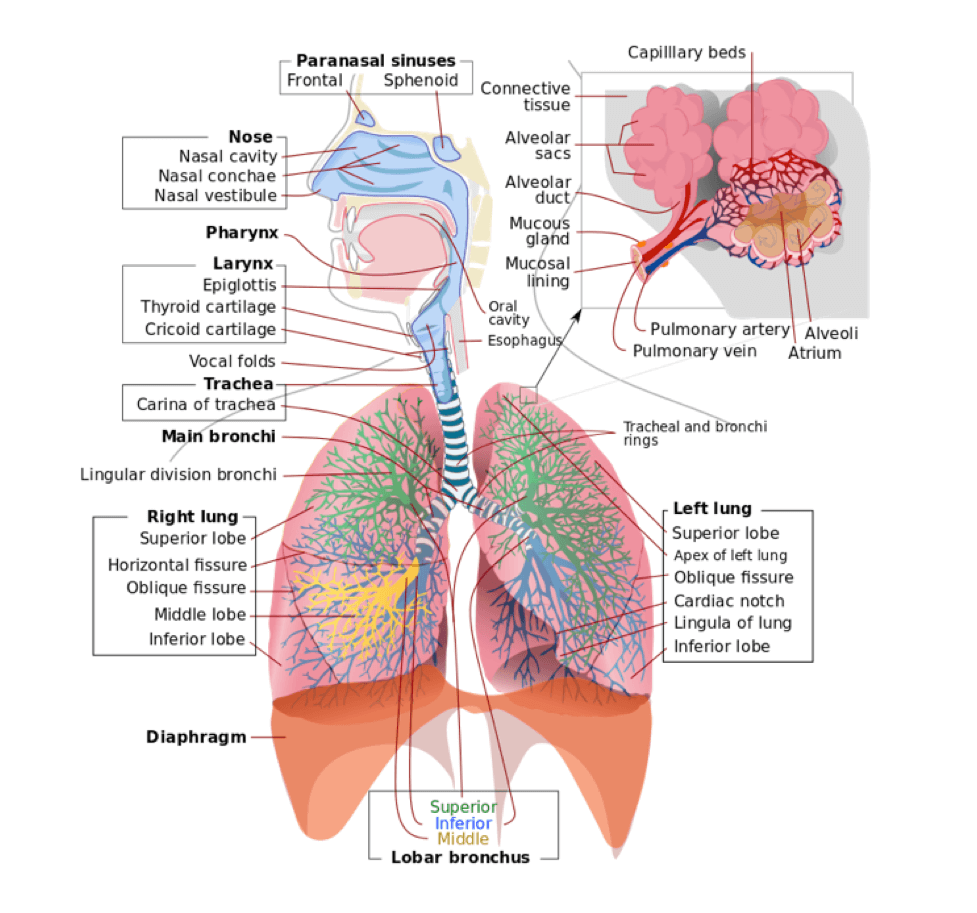
Fig 1. The Anatomy of the Respiratory System
THAT IS A LONG WAY! We can consolidate everything distal to the larynx into cardiac output, vasculature and lung and it’s still a long way. Why is this a problem? I’m going to list them:
- There are more sites for issues along a complex path i.e. more moving parts.
- Look at your friend side on. Look at the angles created between mouth, pharynx, larynx, and tracheobronchial tree. There are at times >90 degree difference between each, often acute angles, bending forwards and immediately backwards. Oxygen must travel from atmosphere, via a partial pressure difference and excellent lung compliance, through a mouth or nose, run parallel to a palate, turn ± 110 degrees back and then ± 70 degrees down, acutely angle behind an epiglottis and immediately bend anteriorly acutely again the enter a larynx. This is assuming a natural airway of an awake patient, no extension or flexion needed… and no anatomical abnormalities obstructing the flow e.g. clefts, trauma, fractures, abscesses, tumors. MAKES YOU THINK HUH? So a fundamental problem is the angles of the various axis, namely oral, pharyngeal and laryngeal axis. These must be aligned, that is made into a straight line in the patient to be intubated. There are no devices, which can bend the way the O2 just did, right? Not so simple anymore.
- Compliance is part of the oxygenator, the volume change for a pressure generated, and it’s not just the lung and pleura, but all tissues. Stiff tissues = poor compliance = problems oxygenating.
- Poiseuille’s Law states flow of fluid (Q) is related to number of factors: viscosity (n), pressure gradient across the tubing (P), length (L) and diameter (r) of the tubing. Q = πP,r-4./8nl. The implications of a change in radius by e.g. A tonsil/hematoma/edema is to decrease flow by the power of 4… this is not to be trifled with. Just look at the next wheezing asthmatic or snoring sleep apnoeic to see the resistance increasing exponentially as the radius decreases.
- We have a small O2 reserve in the functional residual capacity (FRC), which is rapidly depleted in the healthiest patients. Even more so in the sick patient.
- Trauma/ comorbidity worsens every aspect of the pathway.
- Intubation is way overrated as a god-like skill. It’s overemphasized and I guarantee you that unless your patient is obtunded with no airway reflex at all, that your attempts to intubate without pharmacology and paralysis will fail and will cause more trauma than you initially had to deal with.
- EGO… is the hugest obstacle to effectively oxygenating patients. The “I must tube” at all costs to patient and “I’m a doctor step aside” hero mentality is usually morbid and often mortal in outcome. Airways need O2 not EGO2.
- The single most invaluable tool for any doctor is the ability to MASK VENTILATE. If you can’t tube, or place an extraglottic device, you had better still be able to get 02 to through its complicated path to a cell. MASK VENTILATION is the skill of the century. It will keep your patient alive until someone arrives who knows more can help you. It is the only skill you need. Believe me.
- The main job of the oxygenator and you manipulating the oxygenator is for DELIVERING O2, not looking cool or living your Grey’s anatomy dreams.
So how are we to proceed in part 2 of the oxygenator assessment? We are going to look at the 6 big issues that need to be covered from an airway assessment perspective:
- The atmosphere
- Mask ventilation
- Laryngoscopy/intubation → infraglottic
- Rescue airway → supra/extraglottic
- Surgical airway
- Lung compliance
This is by no means a complete treatment of the airway. There are volumes just written on the nasopharynx. This will be a basic introduction, which hopefully you can take with you on one page for the rest of your life. It will be uncomplicated, and filled with mnemonics.
Next: The Oxygenator Assessment – Part 2
Medical Exam Prep would like to thank Dr. Clem Lonnigen Jolly for contributing this post.
About Dr. Clem Lonnigen Jolly
Dr. Clem Lonnigen Jolly is an Anaesthetist working at the Ethekwini Hospital and Heart Centre in KwaZulu-Natal, South Africa
Header image used on licence from Shutterstock





