There are two sittings of the FRCR part 2A exam each year; December and June. There are six different venues within the UK in which the exam can be sat, as well as two overseas venues; Hong Kong and Singapore.
This consists of two papers, each containing 120 single best answer questions, taken on the same day. Each paper lasts for three hours and the scores from both are combined to give a single mark. It is not possible to pass one paper at a time.
Sitting practice questions is a great way to prepare for the FRCR part 2A. Here are a few to get you started.
1. A 45-year-old man with known HIV presents with deteriorating memory problems and word finding difficulties. He undergoes an MRI scan which shows bilateral white matter high signal on T2 and FLAIR in an asymmetric pattern. There is no mass effect. The radiologist notes involvement of the subcortical U-fibres. What is the most likely explanation?
A. Cryptococcus
B. HIV encephalitis
C. Toxoplasmosis
D. Progressive multifocal leukoencephalopathy
E. Cerebral tuberculosis
Show Answer
Progressive multifocal leukoencephalopathy (PML)
This is a JC virus-mediated phenomenon which causes asymmetrical patchy white matter changes. These can be bilateral. The testable feature is involvement of the cortical U-fibres which separates it from HIV encephalopathy where the U-fibres are spared. The lack of a mass effect helps differentiate both PML and HIV encephalopathy from toxoplasmosis, cryptococcus and tuberculomas.
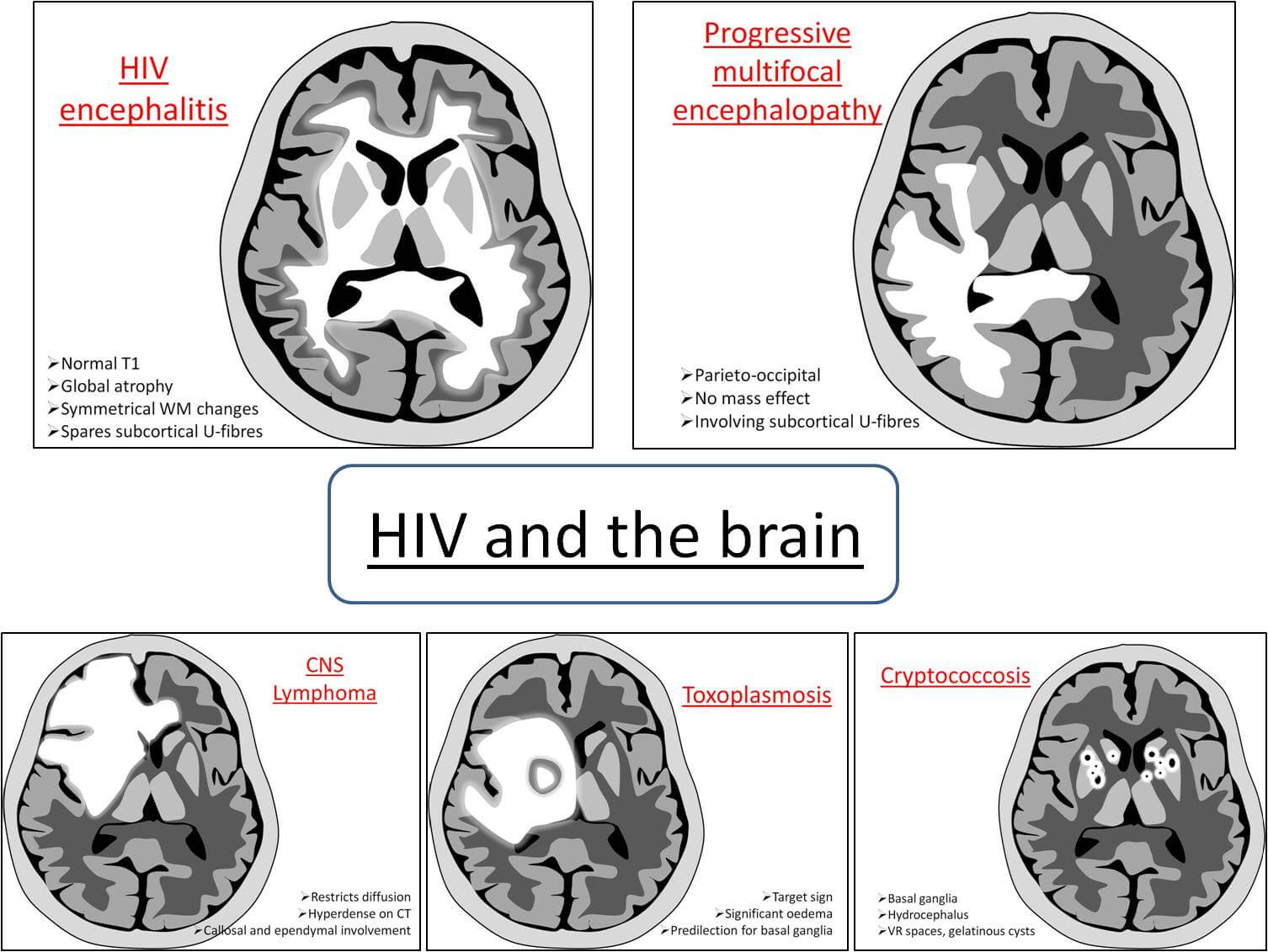
HIV encephalopathy
Separating HIV encephalitis from PML can challenging in real life. HIV encephalitis causes bilateral symmetrical white matter changes, seen as high T2 signal (The T1 sequences can be normal). There is also sparing of the subcortical U-fibres.
Cryptococcus
This is an opportunistic yeast-like fungus which therefore requires a degree of immunocompromise, typically AIDS. The cryptococcomas are non-enhancing low-density lesions in the basal ganglia. These show as high signal on T2 sequences. A granulomatous meningitis can also occur. They can be differentiated from VR spaces on FLAIR where VR spaces will suppress (being CSF in content) whereas the mucoid cryptococcomas will not.
Toxoplasmosis
Toxoplasmosis is a more common finding in AIDS patients than lymphoma is, by a large margin. On MRI it is seen as multiple ring-enhancing lesions, which can show haemorrhage, particularly following treatment. One of the stronger differentiators between toxoplasmosis and lymphoma is the SPECT findings. This is sometimes termed ‘hypometabolic’ meaning the lesions do not demonstrate SPECT uptake. The table below gives some general features of the two conditions. There is however considerable overlap in the imaging features despite these broad trends.
Cerebral tuberculosis
A cerebral tuberculoma would be difficult to differentiate from toxoplasmosis or lymphoma. Classically though they are described as target lesions situated in the corticomedullary regions. They can calcify with treatment which would differentiate them well from other CNS infections.
2. On the ward round of the neonatal intensive care unit a baby is reviewed. She was born four weeks ago at 31+4 weeks gestation. She has been receiving mechanical ventilation but her CXRs have been gradually worsening. The latest one shows hyperinflation of both lungs with coarse linear densities. Focal areas of emphysema can also be seen. There are no pleural effusions. What is the most likely diagnosis?
A. Pulmonary interstitial emphysema
B. Hyaline membrane disease
C. Meconium aspiration
D. Transient tachypnoea of the newborn
E. Bronchopulmonary dysplasia
Show Answer
Of the five main respiratory conditions of the neonate, the differential diagnosis can be narrowed based on gestational age. The presence of hyperinflation can also be useful but may not always be present where feasible so should not be used as an absolute discriminator. If present, it is useful.
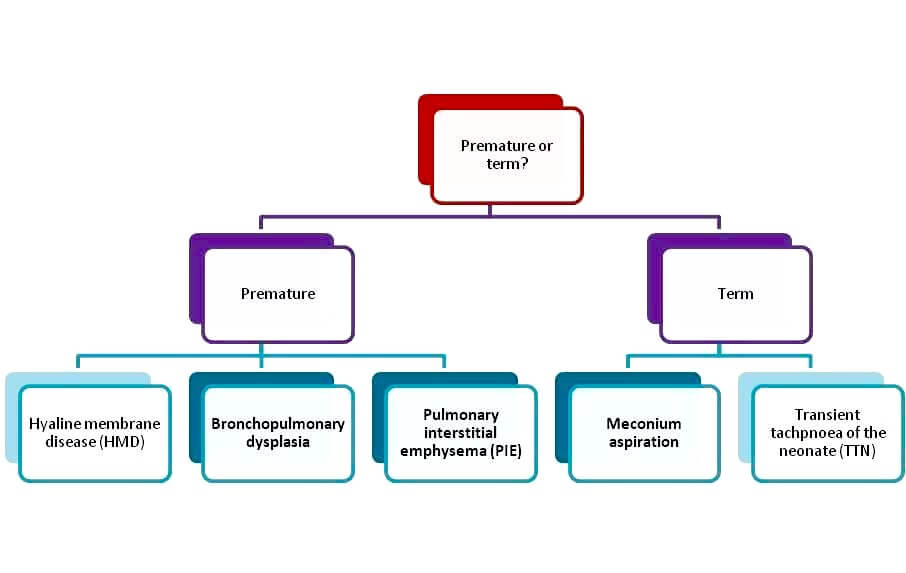
Meconium aspiration
Meconium is sticky and causes a chemical pneumonitis in the lungs, seen as patchy consolidation. In addition small globules of meconium entering bronchi and bronchioles of a decreasing calibre act as a ball-valve mechanism and lead to air trapping; thus the lung volumes of a baby with meconium aspiration may be increased. Air bronchograms are notably absent. The typical baby in a meconium aspiration situation is post-term.
Transient tachypnoea of the newborn (TTN)
The classical patient for TTN would be a term baby born by caesarean section to a diabetic mother. During normal vaginal delivery, the compression of the baby as it descends the birth canal acts to squeeze fluid out from its lungs. This mechanism is all but absent during a caesarean section. Consequently, these babies are born with an excess of retained fluid. The CXR of an affected baby will show bilateral symmetrical airspace opacification with air bronchograms, fluid in the fissures and pleural effusions. This peaks in severity at 24hrs but resolves by three days.
Hyaline Membrane Disease (HMD) also known as surfactant deficient disease (SDD)
It is to reduce the likelihood of this disease developing that a woman in pre-term labour will be offered a steroid injection. The steroids help the neonatal lungs to develop faster and increase the likelihood of their being able to produce surfactant once delivered. Where there is surfactant deficiency the alveoli collapse. The CXR will show a granular opacification throughout both lungs which progresses to bilateral ground-glass opacification with air bronchograms. If exogenous surfactant is given to the baby there may be an asymmetrical improvement in the appearances depending on how much reaches each lung. Of note, HMD does not cause pleural effusions. Finally, a normal CXR at 6hrs post delivery excludes HMD.
Pulmonary interstitial emphysema (PIE)
As the name would suggest, this disease is diagnosed when there is air within the interstitial tissues of the lungs. It is caused by alveolar rupture due to the barotrauma of mechanical ventilation or positive airway pressure. It can be associated with hyaline membrane disease and is prevalent in infants of a low birth weight. Complications such as pneumothorax or pneumomediastinum can be severe and acutely life-threatening. Radiographically there is hyperinflation and lucencies in either a cystic pattern or streaks emanating from the hila and following the direction of the bronchi/bronchioles. It is treated with high-frequency oscillation ventilation which is less traumatic to the lungs.
Bronchopulmonary dysplasia
This also occurs due to barotrauma in ventilated neonates but is a more gradual process, occurring later on in the baby’s life. Typically (but not exclusively) the baby is premature (hence requiring ventilation). It only usually occurs after the baby in question has received ventilation of >21% oxygen for longer than 28 days. The lungs are hyperinflated and what starts off as ground glass opacification becomes complete opacification with air bronchograms in a few days. After 30 days it can be seen as coarse linear lucencies, described as radiating from the hila, with focal emphysematous change. Mikity syndrome has similar features but occurs in term infants who have not received mechanical assistance.
3. A 55-year-old man complains to his GP of pain in both wrists. On examination his GP notices a salmon-pink patch of skin on his forearm. There is some silver coloured scale overlying the patch. Bilateral x-rays of the wrist are requested. Which of the following features would be LEAST likely to be seen?
A. Marginal erosions
B. Osteoporosis
C. Soft tissue swelling
D. Pencil-in-cup deformity
E. Periosteal reaction
Show Answer
Psoriatic arthropathy
Around a fifth of patients with psoriasis develop arthropathy and it is also possible to suffer from psoriatic arthropathy in the absence of the typical psoriatic cutaneous plaques.
Importantly, on x-ray, there are findings of both erosive changes in addition to productive changes with periosteal new bone formation. The combination of the two contrives to leave a ‘pencil-in-cup’ appearance. The joints can appear fluffy due to the exuberance of new bone formation. The differential diagnosis for periosteal reactions in the presence of an arthropathy is relatively narrow and very specific (see below).
Periosteal reaction + arthropathy:
- Psoriatic arthropathy
- Juvenile Rheumatoid arthritis
- Reiter syndrome
- Infective arthropathy
Although often classified as a distal arthropathy, preferring the DIPs to the MCPs, psoriatic arthropathy does also affect the spine and SI joints frequently. ‘Sausage digits’ is a term used to describe the diffuse soft tissue swelling which can affect the fingers and toes. Osteoporosis does occur but is a feature of later disease.
4. A 76-year-old farmer is undergoing a cardiac MRI for investigation of dyspnoeic symptoms. There is nodular pericardial thickening which shows high signal on T1 and low on T2 associated with a small pericardial effusion. What is the most likely diagnosis?
A. Mycobacterium Avium Intracellulare
B. Extrinsic Allergic Alveolitis
C. Renal cell carcinoma metastasis
D. Lung cancer metastasis
E. Melanoma metastasis
Show Answer
MRI is seldom used in the world of pulmonary radiology. Nonetheless, the physics is the same throughout the body in that there are a limited number of entities which show high signal on T1.
These are the 4Ms and the 3Fs, thus:
- Melanin
- Methaemoglobin (subacute haemorrhage)
- Mineralisation (manganese, copper)
- Magnevist (gadolinium contrast agents)
- Fluid – proteinaceous (N.B posterior pituitary stores anti-diuretic hormone and is therefore bright)
- Fat
- Flow – slow
Arguably renal cell carcinoma metastases could cause high T1 signal since they can show haemorrhage however the clinical information in the question alludes to the patient having occupational exposure to sunlight predisposing him to melanoma formation.
5. Which MRI features are most likely to represent a malignant breast lesion? Select ONE answer only.
A. Early contrast enhancement
B. Spiculations
C. Bright on T1
D. Popcorn calcification
E. Slow contrast enhancement
Show Answer
In a nutshell ‘morphology trumps kinetics’ for breast MRI. That is to say that if a lesion is suspicious on morphology, even if the kinetics are normal it should be treated as a suspicious lesion. Suspicious kinetics would constitute fast uptake and fast washout, such as in early contrast enhancement. Spiculations in any modality are suspicious because they represent the desmoplastic reaction of the normal breast tissue surrounding a malignant lesion. Popcorn calcifications are classical for benign fibroadenomas.





It’s very nice and very informative
Wow that’s powerful Very informative
Very nice cases how can I a regular member for Frcr?
Hi Dr Ikram – thank you for the feedback. You can sign up for all of our FRCR cases and questions here: https://www.frcrexamprep.co.uk/store/final-frcr-part-2a
Good attempt at brain storming
Very beautiful. A nice attempt at stimulating residents for both local and international exams
Thanks 😊😊
Quite informative questions.
👍👍👍
Very informative and refreshing for everyone
very effective
I need more of this to build my career
Mesmerising. So much to learn.
Thank you!
Excellent and very informative.
Much informative. Learnt a lot.
I find this very helpful.
I find this very informative and useful. I wish to read this every day. This is a must read material for residents and a handy refrence for consultants wishing to refresh their memories.