Puberty is the process by which a child’s body matures into an adult body and becomes capable of sexual reproduction. It is a complex process involving both physical growth and sexual and psychosocial maturation.
Puberty usually begins between 8 and 14 years of age in girls and 9 and 14 years in boys. Data from the USA indicate that onset of puberty has been gradually becoming slightly earlier, both in boys and in girls.
Hormonal changes during puberty
The process of puberty is controlled by the hormones of the hypothalamic-pituitary-gonadal (HPG) axis. The hypothalamus releases gonadotropin-releasing hormone (GnRH) in a pulsatile manner. The anterior pituitary gland responds to the pulsed GnRH signals by releasing follicle-stimulating hormone (FSH) and luteinising hormone (LH).
In turn, the gonads (the ovaries in females and the testes in males) respond to rising levels of FSH and LH to stimulate by releasing the sex steroid hormones (oestrogen and progesterone in females and testosterone in males). FSH and LH exert many effects on the reproductive system and have a negative feedback effect on the hypothalamus and the pituitary gland, ensuring that circulating levels remain stable.
FSH and LH levels are low throughout childhood, possibly due to the slow cycling of the GnRH pulse generator in the hypothalamus. About a year before the first physical changes of puberty can be seen; there is an increase in the pulsatile release of FSH and LH from the anterior pituitary. This is thought to be due to the removal of central nervous system inhibition of the GnRH pulse generator.
Rising FSH levels stimulate an increase in oestrogen synthesis and oogenesis in females and the commencement of sperm production in males. Rising LH levels stimulate an increase in progesterone production in females and an increase in testosterone production in males. These hormonal changes result in the onset of characteristic physical changes associated with puberty.
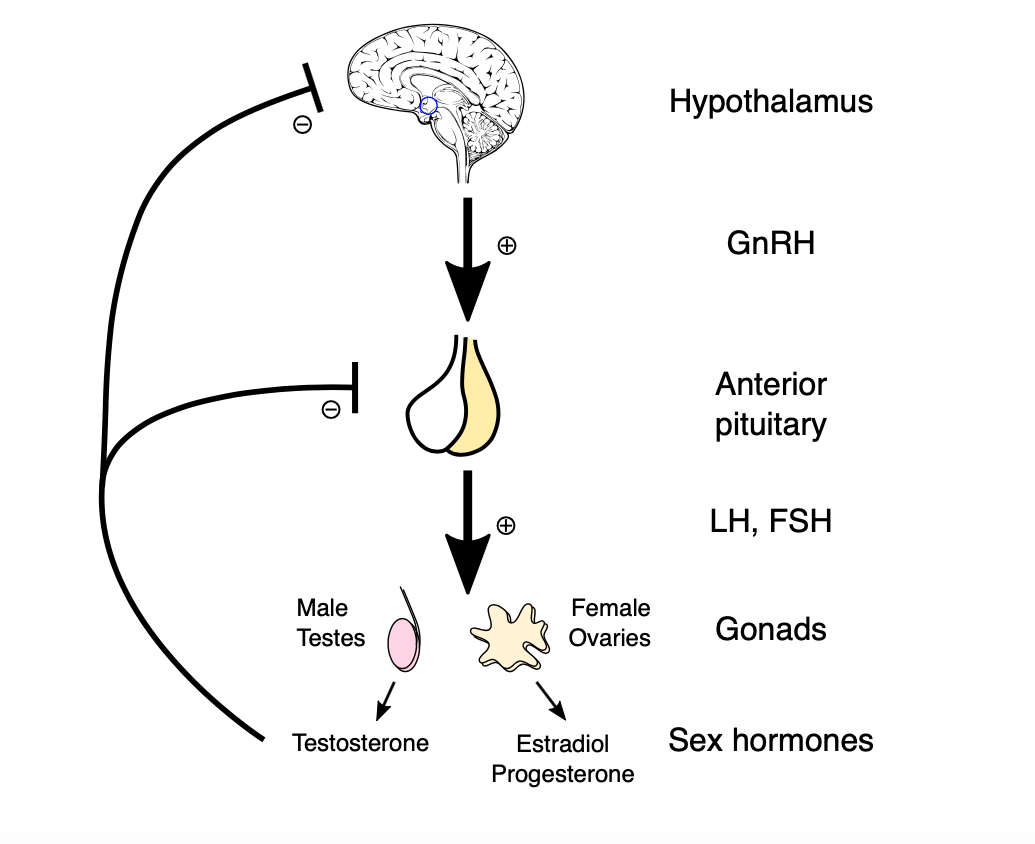
The HPG axis, image sourced from Wikipedia
Courtesy of Artoria2e5 CC BY-SA 3.0
The Tanner scale
The Tanner scale is one of the most commonly used measurement scales of sexual maturity. It was developed by the British paediatrician James Tanner in 1969, following a two-decade-long study that followed the physical changes in girls undergoing puberty.
The Tanner scale defines the physical measurements of development based on external primary and secondary sexual characteristics, such as breast size, testicular volume and pubic hair development.
Normal puberty in girls
The most common initial sign of puberty in girls is breast development (thelarche). This usually commences between the ages of 8 and 14. 50% of girls in the UK will have developed breast buds by the age of 11, and near-full breast development will have occurred in 50% of girls by age 13.
Menarche usually occurs around two to three years after thelarche. In the UK, the average age of menarche is approximately 13 years. The growth spurt occurs earlier in female puberty. It is usually maximal (about 8 cm/year) during Tanner’s breast stages 2 and 3. and reduces to 4 cm/year at menarche. The average duration of puberty in girls is 2.7 years.
The following table summarises the Tanner stages of development in girls:
| Tanner stage | Breasts | Pubic hair | Growth | Other features |
|---|---|---|---|---|
| Stage 1 | Prepubertal - elevation of papilla only | Prepubertal - villus hair only | Basal level - 5 cm to 6 cm per year | Adrenarche Ovaries grow and enlarge |
| Stage 2 | Breast bud appears under an enlarged areola (mean age 11.2 years) | Sparse hair appears along the labia (mean age 11.9 years) | Accelerated growth – 7 cm to 8 cm per year | Clitoral enlargement Labial pigmentation Uterine enlargement |
| Stage 3 | Breast tissue grows beyond areola but without contour separation (mean age 12.4 years) | Hair coarser and pigmented – spreads across pubes (mean age 12.7 years) | Peak velocity – 8 cm per year (mean age 12.5 years) | Axillary hair Acne development |
| Stage 4 | Projection of areola – papilla forms a secondary mound (mean age 13.1 years) | Adult pattern but without spreads to the medial thigh (mean age 13.4 years) | Deceleration – less than 7 cm per year | Menarche (mean age 13.3 years) Regular periods (mean age 13.9 years) |
| Stage 5 | Adult breast contour with projection of papilla (mean age 14.5 years) | Adult pattern with spread to the medial thigh (mean age 14.6 years) | Cessation of growth at around 16 years | Adult genitalia |
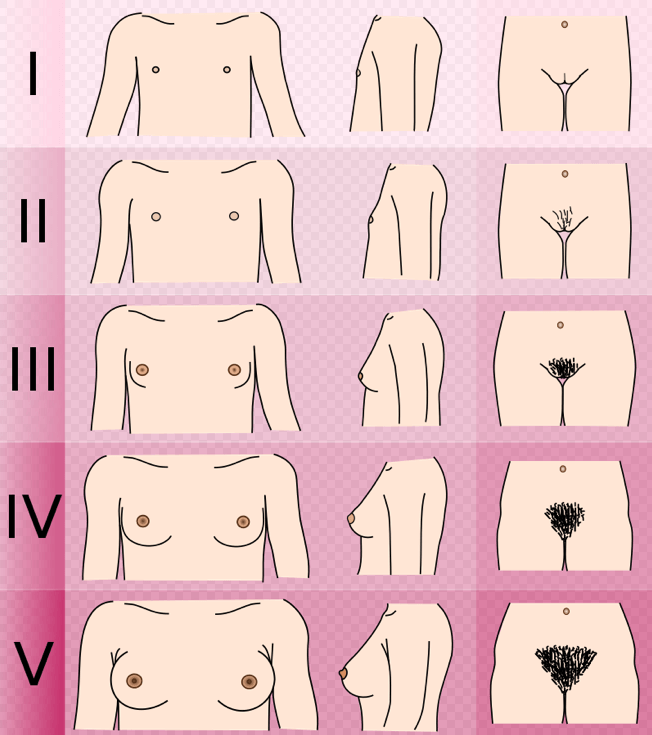
Visual summary of the Tanner scale in girls, image sourced from Wikipedia
Courtesy of Michael Komorniczak (Poland) CC BY-SA 3.0
Normal puberty in boys
The first apparent physical sign is testicular enlargement between the age of 10 and 13 years of age, but this is subtle and often goes unnoticed. The prepubertal testis is approximately 2 ml in volume, and the onset of puberty is indicated by a rise in volume to 4 ml. Penile and scrotal enlargement usually occurs around a year after the commencement of testicular enlargement. Spermatozoa become present in early morning urine samples at about 13 and a half years of age (spermarche).
The growth peak in boys occurs around two to three years later than in girls. Other signs include the development of facial hair, the appearance of acne, and the deepening of the voice.
The following table summarises the Tanner stages of development in boys:
| Tanner stage | Genitalia | Pubic hair | Growth | Other features |
|---|---|---|---|---|
| Stage 1 | Prepubertal – testes less than 2.5 cm | Prepubertal - villus hair only | Basal level - 5 cm to 6 cm per year | Adrenarche |
| Stage 2 | Thickening and reddening of scrotal skin (mean age 11.9 years) Testes 2.5 cm to 3.2 cm | Sparse hair growth at the base of the penis (mean age 12.3 years) | Basal level unchanged - 5 cm to 6 cm per year | Reduction in total body fat |
| Stage 3 | Growth of penis (mean age 13.2 years) Testes 3.3 cm to 4 cm | Thicker hair – spreads to mons pubis (mean age 13.9 years) | Accelerated growth – 7 cm to 8 cm per year | Gynaecomastia Voice break Increase in muscle mass |
| Stage 4 | Growth of penis and glans with darkening of the scrotum (mean age 14.3 years) Testes 4.1 cm to 4.5 cm | Adult pattern but without spreads to medial thigh (mean age 14.7 years) | Peak velocity – 10 cm per year (mean age 13.8 years) | Axillary hair Voice change Acne development |
| Stage 5 | Adult genitalia (mean age 15.1 years) Testes greater than 4.5 cm | Adult pattern with spread to the medial thigh (mean age 15.3 years) | Deceleration and cessation of growth at around 17 years | Facial hair Further increase in muscle mass |
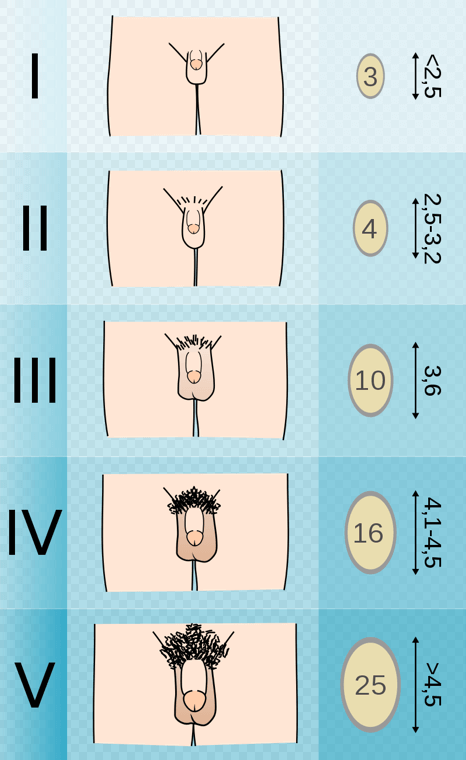
Visual summary of the Tanner scale in boys, image sourced from Wikipedia
Courtesy of Michael Komorniczak (Poland) CC BY-SA 3.0
Precocious puberty
Precocious puberty is defined as the appearance of secondary sexual characteristics before the age of 8 in girls or before 9 in boys. Precocious puberty can be further subdivided as follows:
- Isosexual – precocious puberty with phenotypically appropriate secondary sexual characteristics
- Heterosexual (or contrasexual) – precocious puberty with the development of characteristics of the opposite sex, e.g. feminisation of a male or virilisation of a female (rare compared to isosexual precocious puberty.
The possible causes of precocious puberty include the following:
- Idiopathic – no cause is found in 80% of girls and 40% of boys
- True – due to early maturation of the HPG axis resulting in high levels of GnRH, FSH and LH. This is usually due to abnormalities of the central nervous system, such as brain tumours, trauma, hypothalamic hamartomas and congenital disorders (e.g. hydrocephalus and arachnoid cysts)
- Peripheral – gonadotropin-independent precocious puberty. This can be caused by specific rare genetic syndromes, ovarian or testicular tumours and disorders of the adrenal gland
- Iatrogenic – due to exposure to exogenous oestrogens, e.g. via creams or lotions etc.
Delayed or absent Puberty
Delayed or absent puberty is defined as the absence of secondary sexual characteristics by the age of 13 in girls or 16 in boys.
The possible causes of delayed or absent puberty include the following:
Hypogonadotropic hypogonadism – due to disorders of either the hypothalamus or the pituitary gland, resulting in a deficiency of GnRH, LH or FSH.
Hypergonadotropic hypogonadism – due to disorders of the ovaries in girls or testes in boys. This results in absent or reduced gonadal steroid secretion, which, in turn, results in high circulating levels of LH and FSH due to a loss of negative feedback from the gonadal steroids on the pituitary gland.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this article.