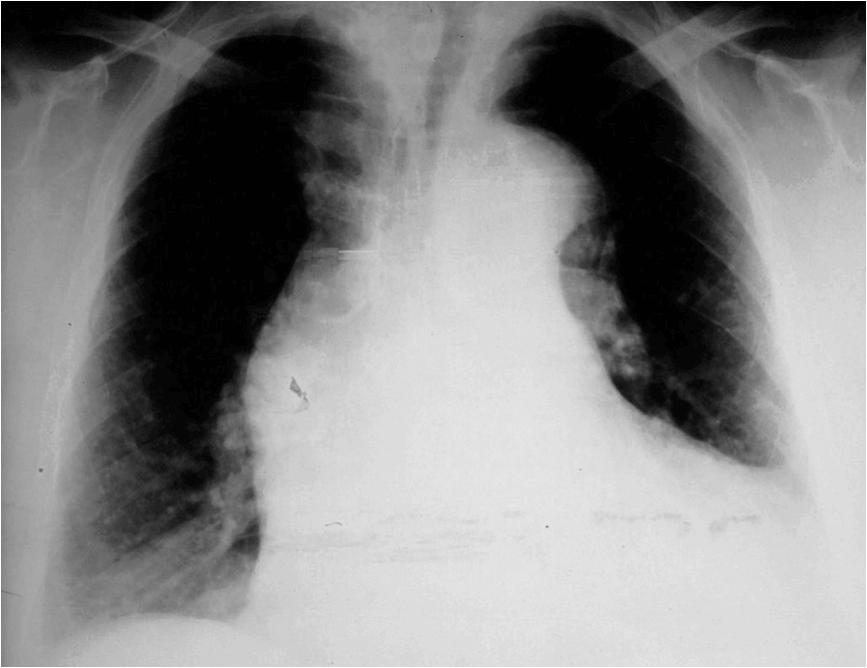
A 38-year-old man with Marfan syndrome presents with sudden severe chest pain that radiates through to his back. He describes the pain as being sharp and ‘ripping’ in nature. He smokes 25 cigarettes per day. He is sweaty, nauseated and appears pallid. On examination you note the presence of an early diastolic murmur. A chest X-ray is performed, which is shown below:
Show Answer
This patient has an acute aortic dissection. Acute aortic dissection is defined as the rapid development of a false, blood-filled channel within the tunica media of the aorta. It has an estimated incidence of 3 per 100,000 persons per year.
Patients with aortic dissection typically present with severe central chest pain that radiates through to the interscapular area. The pain is often described as being ‘tearing’ or ‘ripping’ in nature and may also radiate into the neck. Sweating, pallor and tachycardia are all also commonly seen at presentation. Other features that may be present include focal neurological deficits, pulse deficits, syncope and end organ ischaemia.
An inter-arm blood pressure differential of greater than 20 mmHg is a highly sensitive predictor. Retrograde extension can involve the aortic valve resulting in the appearance of the early diastolic murmur of aortic regurgitation.
Chest X-ray sourced from Wikipedia
Courtesy of J. Heuser CC BY-SA 3.0
Show Answer
This patient has Marfan syndrome, which is a recognized risk factor for the development of aortic dissection. Marfan syndrome causes progressive enlargement of the aortic root, which can predispose to dissection in the ascending aorta. Marfan syndrome is present in 5-9% of patients who suffer aortic dissection.
Other risk factors include:
- Hypertension
- Atherosclerosis
- Aortic coarctation
- Sympathomimetic drug use e.g. cocaine
- Ehlers-Danlos syndrome
- Turner’s syndrome
- Tertiary syphilis
- Pre-existing aortic aneurysm
Show Answer
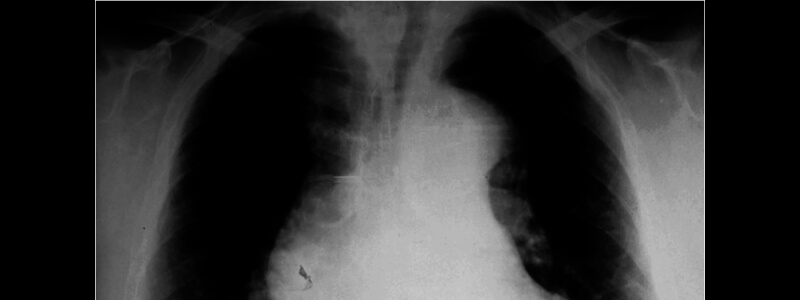
This chest X-ray demonstrates a widened mediastinum, which is one of the commonest chest X-ray findings in aortic dissection.
Other chest X-ray changes that are frequently present include the following:
- Wide aortic knob (seen in this case)
- Double aortic contour
- Irregular aortic contour
- Depression of left mainstem bronchus
- Loss of paratracheal stripe
- Tracheal deviation
Chest X-ray alone has inadequate sensitivity and specificity to completely exclude or confirm the diagnosis and a CT scan or MRI scan should be performed if the diagnosis is suspected.
The CT scan shown below demonstrates aneurismal dilatation and a dissection of the ascending aorta:
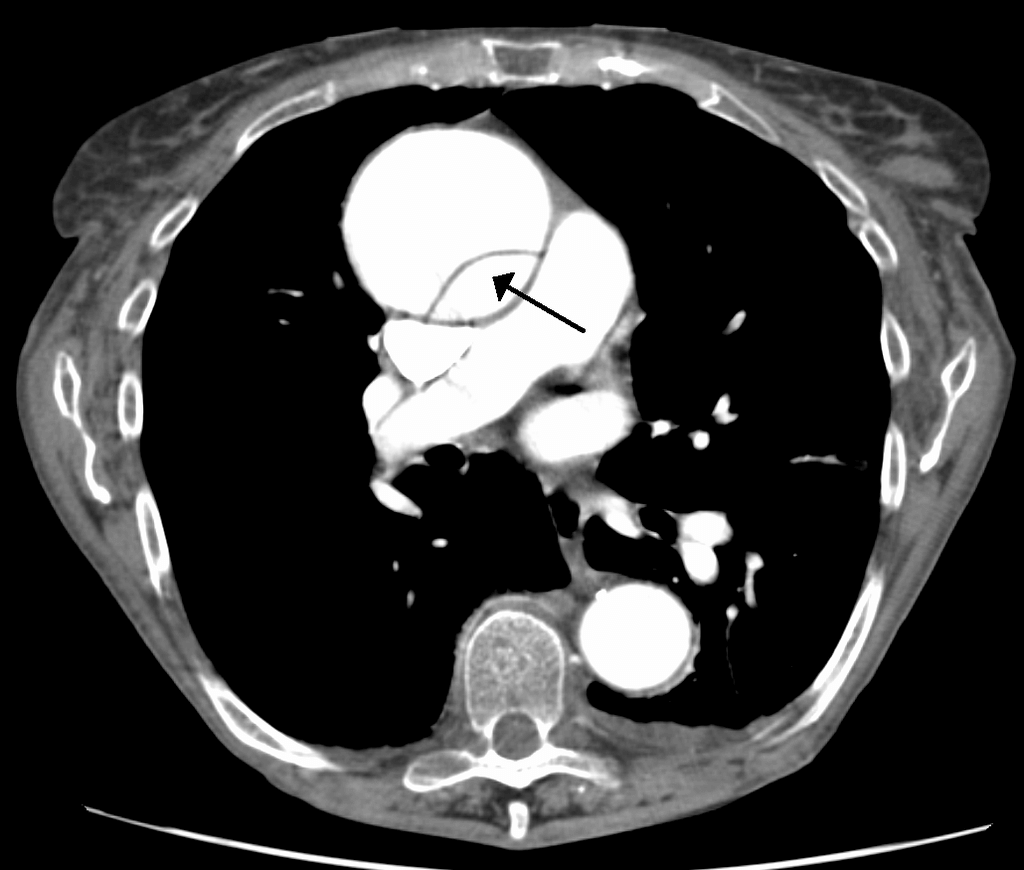
CT scan sourced from Wikipedia
Courtesy of James Heilman CC BY-SA 3.0
Show Answer
Aortic dissection can be classified by either using the Stanford classification or the DeBakey system.
The Stanford classification divides dissections into two groups; A and B depending upon whether the ascending aorta is involved:
1. Type A – affects the ascending aorta and the arch and accounts for 60% of dissections. These are generally managed surgically and may result in coronary artery occlusion and aortic regurgitation.
2. Type B – dissection commences distal to the left subclavian artery and accounts for approximately 40% of dissections. These are generally managed medically with blood pressure control.
The DeBakey system describes the dissections anatomically and categorizes them into three groups:
1. Type I – originates in the ascending aorta, propagates at least to the aortic arch and often beyond it distally (most lethal form)
2. Type II – originates in the ascending aorta and is confined to the ascending aorta
3. Type III – originates in the descending aorta, rarely extends proximally but will extend distally





These cases, are really well presented, what great cpd/reflection pieces.
Thank you
Scott
Thank you Scott