Sympathomimetic drugs are stimulant compounds that mimic the effects of endogenous agonists of the sympathetic nervous system. These drugs are used in a variety of situations, including cardiac arrest, haemorrhage, sepsis and myocardial insufficiency.
Mechanism of action
Sympathomimetic drugs work by stimulating adrenergic receptors, a class of G protein-coupled receptors that receive neuronal impulses from postganglionic adrenergic fibres of the sympathetic nervous system.
Adrenergic receptors are divided into alpha and beta receptors. Sympathomimetic drugs cause vascular smooth muscle contraction and vasoconstriction by activating alpha-adrenergic receptors and stimulate the heart, having a positive inotropic effect by activating beta-adrenergic receptors.
Each sympathomimetic drug has varying activity on the alpha- and beta-adrenergic receptors. They are classified as either inotropic or vasoconstrictor sympathomimetics, depending upon the predominant action.
Vasoconstrictor sympathomimetics include:
- Adrenaline (epinephrine)
- Noradrenaline (norepinephrine)
- Ephedrine
- Metaraminol
Inotropic sympathomimetics include:
- Dopamine
- Dobutamine
- Isoprenaline
Table summarising the location and action of the alpha- and beta-adrenergic receptors:
| Receptor | Location | Action |
|---|---|---|
| Alpha-1 | Vascular smooth muscle | Vasoconstriction and increased peripheral resistance |
| Alpha-2 | Central and peripheral nervous system | Inhibits the release of noradrenaline |
| Beta-1 | Myocardium | Increased myocardial contractility, tachycardia and release of renin from the juxtaglomerular apparatus of the kidney |
| Beta-2 | Bronchial and vascular smooth muscle | Vasodilatation of bronchioles and peripheral vessels causing decreased peripheral resistance |
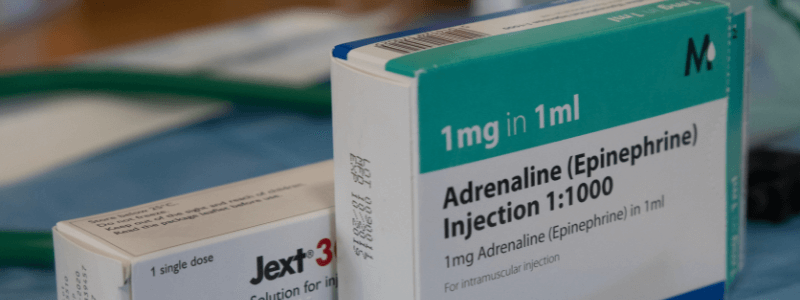
Adrenaline
Adrenaline (epinephrine) acts on both alpha- and beta-adrenergic receptors. The alpha-adrenergic effects of adrenaline cause systemic vasoconstriction, which increases coronary and cerebral perfusion pressures. The beta-adrenergic effects of adrenaline are positively inotropic (increased myocardial contractility) and chronotropic (increased heart rate) and may increase coronary and cerebral blood flow. The two main uses of adrenaline are cardiopulmonary resuscitation and anaphylaxis.
The doses in cardiopulmonary resuscitation are as follows:
- Adults – IV/IO dose of 1 mg IV every 3-5 minutes as required
- Children – IV/IO dose of 10 mcg/kg every 3-5 minutes as required
- 1:10,000 (100 mcg/mL) solution is recommended
The age-related doses of IM adrenaline given in anaphylaxis are:
- Child under 6 years: 150 mcg (0.15 mL of 1:1000)
- Child 6-12 years: 300 mcg (0.3 mL of 1:1000)
- Child over 12: 500 mcg (0.5 mL of 1:1000)
- Adult: 500 mcg (0.5 mL of 1:1000)
Noradrenaline
Noradrenaline (norepinephrine) acts mainly on alpha-1-adrenergic receptors with few effects on beta receptors, causing an increase in blood pressure. It is less likely to cause tachycardia than adrenaline because of its lesser effect on beta-adrenergic receptors. Noradrenaline is primarily used in the treatment of hypotension and shock.
Noradrenaline is usually administered by intravenous infusion at an initial dose of 0.16–0.33 mL/minute, adjusted according to response (solution containing noradrenaline 40 micrograms(base)/mL).
Dopamine
Dopamine is a naturally occurring catecholamine used in the management of low cardiac output states, septic shock, and renal failure. It is the immediate precursor of both adrenaline and noradrenaline.
At low doses (1-5 μg/kg/min), dopamine acts upon D1 and D2 dopamine receptors in the renal, mesenteric and coronary beds. At these doses, dopamine causes a marked decrease in renal vascular resistance and increases renal blood flow. It is also involved in the central modulation of behaviour and movement within this dose range.
At higher dose ranges, dopamine acts via direct and indirect stimulation of beta- and alpha-adrenergic receptors. At an infusion rate of 5-10 μg/kg/min, beta-stimulation predominates, which results in a positive inotropic effect, increasing cardiac output and coronary blood flow.
At infusion rates exceeding 15 μg/kg/min, alpha-stimulation predominates, which results in peripheral vasoconstriction, leading to an increase in venous return and systolic blood pressure.
There is a marked variability in clearance in critically ill patients; therefore, plasma concentrations cannot be reliably predicted from infusion rates.
Dopamine is administered via an intravenous infusion, and because extravasation may result in sloughing and tissue necrosis, a central line is generally preferred (particularly at higher doses >240 μg/min). However, in emergency cases, dopamine may be given peripherally using a large vein (cephalic or basilic) while a central line is prepared. It is inactivated by alkaline intravenous solutions and should not be infused with a sodium bicarbonate solution.
The main side effects of dopamine are:
- Nausea and vomiting
- Tachycardia
- Dysrhythmias
- Angina
- Hypertension
Dobutamine
Dobutamine is a synthetic isoprenaline derivative used to provide inotropic support in patients with low cardiac output due to septic shock, myocardial infarction, and other cardiac conditions.
Dobutamine is a directly acting sympathomimetic whose primary activity results from the stimulation of beta-1-adrenergic receptors in the heart. It, therefore, has positively inotropic effects, increasing cardiac contractility and cardiac output. It also has some weak alpha1-adrenergic and beta-2-adrenergic activity.
It is infused intravenously diluted in a suitable crystalloid solution to a volume of at least 50 ml. The dose range is 0.5-40 μg/kg/min, titrated to response. Skin necrosis due to extravasation is rare, and dobutamine may be given via a peripheral line.
Side effects are uncommon at dose ranges below 10 μg/kg/min, but at higher doses, the following can occur:
- Nausea and vomiting
- Tachycardia
- Dysrhythmias
- Angina
- Hypertension
- Headache
Summary
A summary of the mechanism and effects of different inotropic agents is shown in the table below:
| Inotrope | Mechanism | Effects |
|---|---|---|
| Adrenaline (epinephrine) | Beta-1 and -2 agonist at increasing doses; Alpha-agonist at high doses | Increased cardiac output; Vasoconstriction at higher doses |
| Noradrenaline (norepinephrine) | Mainly alpha-agonist; Beta-1 and -2 agonist at increasing doses | Vasoconstriction; Some increased cardiac output |
| Dopamine | Dopamine agonist at low doses; Beta-1 and -2 agonist at increasing doses; Alpha-agonist at high doses | Increased cardiac output; Vasoconstriction at higher doses |
| Dobutamine | Mainly beta-1 agonist | Increased cardiac output |
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcemexamprep.net for this ‘Exam Tips’ blog post.