Lyme disease is caused by the spirochete bacterium Borrelia burgdorferi. It is transmitted to humans through the bite of infected Ixodes spp. ticks. In high-risk areas, it is estimated that as many as 40% of ticks can be infected.
The incidence of Lyme disease is steadily increasing in the UK and Europe, and this is possibly due to the effects of global warming allowing the ticks spread to higher altitudes and more northern latitudes. Particularly high-risk areas in the UK are the South of England and the Scottish Highlands, but the disease is now endemic in the UK. The ticks are most commonly found in grassy and wooded areas, including urban gardens and parks.
Clinical features of Lyme disease
Some of those infected will be entirely asymptomatic and may not even recall the causative tick bite. The presentation is variable and depends upon the stage of disease, but the erythema chronicum migrans is the earliest and most consistent sign and is considered to be pathognomic for Lyme disease.
Stage 1 disease (early Lyme disease):
The only symptom in stage 1 is the erythema chronicum migrans rash. This occurs in about 75-85% of patients that have Lyme disease. It starts as a red macule or papule that appears at the site of the tick bite and then radiates out as a red circular rash developing a ‘bullseye’ appearance. It can present 3-30 days after being bitten and is very distinctive. Commonly affected areas include the popliteal fossa, groin, the axilla, the thorax and the trunk. The hairline and scalp are especially common in children.

The classic erythema chronicum migrans rash (image used on licence from Shutterstock)
Stage 2 disease (early disseminated Lyme disease):
If left untreated, disseminated infection follows the rash. The disseminated stage is still considered to be early infection and usually occurs within a few days to a few weeks of the rash appearing (but can occur several months later). Typical symptoms and signs seen in this stage include:
- A flu-like illness with fever, myalgia, arthralgia, lymphadenopathy, headache, fatigue, and nausea or vomiting.
- Neurological problems (neuroborreliosis) – unilateral or bilateral facial nerve palsies are the most common neurological manifestation. Meningism, meningitis and encephalitis can occur more rarely.
- Cardiovascular problems – myopericarditis and heart blocks can occur rarely.
- Lymphocytomas – bluish-red nodular lesions infiltrated with lymphocytes, usually seen on the nipple or earlobe.
Stage 3 disease (late disseminated Lyme disease):
The late-stage occurs in untreated patients several months after the initial infection. The clinical features seen in this stage include:
- Large joint arthritis, most commonly affecting the knee joint. Can be relapsing and remitting or, more rarely chronic and progressive.
- Late neurological problems – including chronic encephalomyelitis, polyneuropathy and psychiatric disorders.
- Acrodermatitis chronica atrophicans – this very rare and can occur years after the initial infection. It is characterised by a red-blue discolouration and swelling on the extensor surface of a limb.
Investigation of Lyme disease
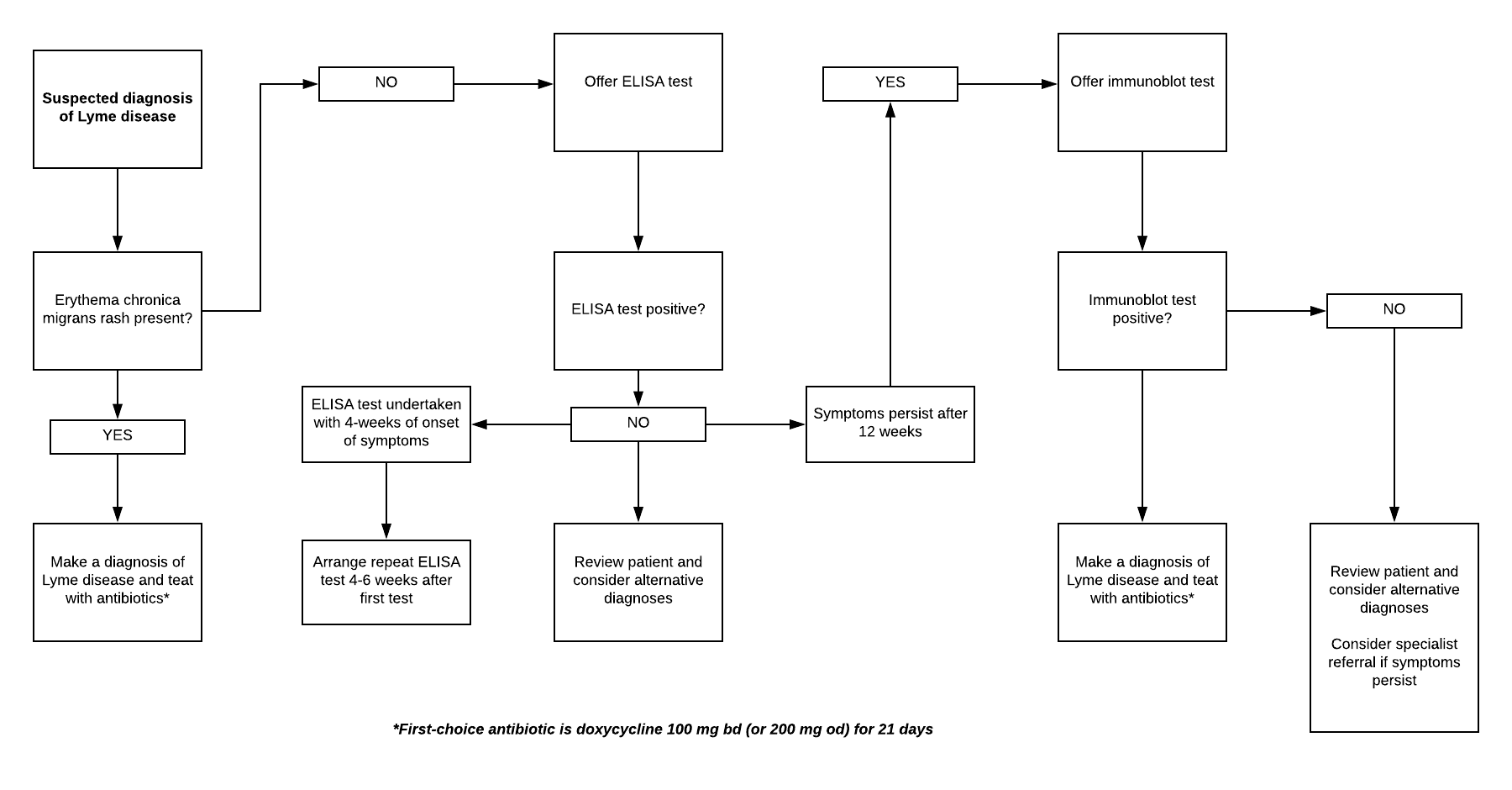
The current NICE guidelines on Lyme disease recommend that a diagnosis of Lyme disease can be made clinically in patients with the erythema chronicum migrans rash. In patients without the rash, a combination of clinical judgement and laboratory testing should be used.
In patients with a clinically suspected diagnosis, but no rash, the first-line test of choice is the enzyme-linked immunosorbent assay (ELISA) test for Lyme disease. NICE recommends that treatment with antibiotics should be considered while awaiting the test results.
If the ELISA test is positive or equivocal an immunoblot test for Lyme disease should be performed, and antibiotics should be considered if the patient has not already commenced treatment.
If Lyme disease is still suspected in patients with a negative ELISA who were tested within 4 weeks from symptom onset, the ELISA test should be repeated 4-6 weeks later. If Lyme disease is still suspected in people with a negative ELISA who have had symptoms for 12 weeks or more, then an immunoblot test should be undertaken. If the immunoblot test for Lyme disease is negative (regardless of the ELISA result), but symptoms persist, then a specialist referral should be considered.
The pathway below is adapted from the NICE visual summary of the recommendations on testing for Lyme disease:
Management of Lyme disease
Patients with symptoms suggestive of central nervous system infection, cardiovascular complication or uveitis should be referred as an Emergency to secondary care.
NICE recommend the following antibiotics regimens for the treatment of Lyme disease:
- First-choice – oral doxycycline 100 mg bd (or 200 mg od) for 21 days
- Second-choice – oral amoxicillin 1 g tds for 21 days
- Third-choice – oral azithromycin 500 mg od for 17 days
If intravenous antibiotics are needed (e.g. for Lyme carditis or arthritis), then the recommended antibiotic is IV ceftriaxone 2 g od for 28 days.
Further reading:
NICE Clinical Knowledge Summary on the management of Lyme disease
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this article.






Excellent up to date