Eosinophilic oesophagitis, which is sometimes abbreviated to EoE in American publications, is an allergic inflammatory condition of the oesophagus that involves eosinophils. It was first discovered as a clinical entity around 20 years ago but has only recently become recognised on a broader scale.
Eosinophilic oesophagitis is associated with allergic disease but is not caused by a classic IgE-mediated response. Instead, it is driven by T-helper type-2 cells. These release a range of cytokines in response to trigger allergens resulting in eosinophilic recruitment in the oesophagus and subsequent mast cell activation. Histamine and transforming growth factor beta cause chronic inflammation, fibrosis and reduced contractility.
Epidemiology of eosinophilic oesophagitis
Eosinophilic oesophagitis occurs most commonly in middle age (average age at diagnosis is 30-50 years). It is more common in men with a 3:1 male-to-female ratio is 3:1. It is commonly associated with allergic conditions, in particular, atopy.
Prevalence has increased in recent years, but it is not known if this is due to improved awareness and diagnosis of the condition, or whether this is a genuine increase. A community study in Sweden reported a prevalence of 4 in 10,000. A UK general practice should expect to have one patient with eosinophilic oesophagitis for every 2,500 patients on its list. The oesophageal section of the British Society of Gastroenterology set up a National Registry in March 2010. 300 patients were registered in the first 18 months.
Clinical features of eosinophilic oesophagitis
The clinical features of eosinophilic oesophagitis depend upon the age of the patient.
Adults tend to present with the following features:
- Dysphagia
- Food bolus obstruction
- Heartburn
- Chest pain
Children tend to present with the following features:
- Failure to thrive
- Food refusal and difficulty feeding
- Vomiting
- Abdominal pain
The key to diagnosis is in considering the possibility of eosinophilic oesophagitis in patients presenting with persistent heartburn and/or difficulty swallowing in patients with a history of allergy or atopic disease.
Diagnosis of eosinophilic oesophagitis
Diagnosis relies on demonstrating more than 15 eosinophils per high-power field on microscopy of an oesophageal biopsy. Allergy testing is ineffective as the condition is not IgE-mediated.
Endoscopic abnormalities of the oesophagus include the following:
- Diminished vascular pattern
- Mucosal furrows
- Thick mucosa
- Exudates
- Strictures
- Concentric rings (trachealisation of the oesophagus)
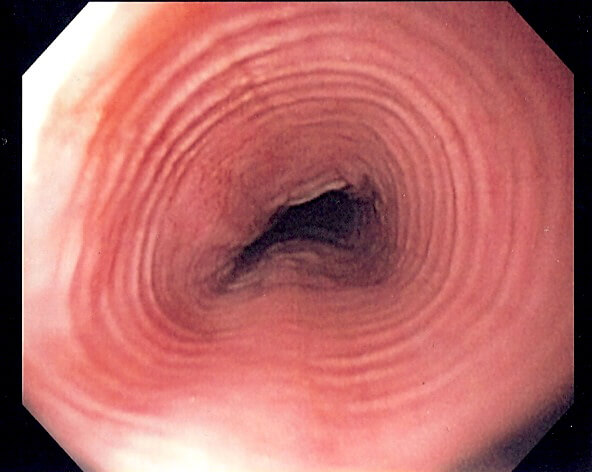
Trachealisation of the oesophagus in a patient with eosinophilic oesophagitis, image sourced from Wikipedia
Courtesy of Samir CC BY-SA 3.0
Management of eosinophilic oesophagitis
There are three main management options for patients with eosinophilic oesophagitis. At this point, all three are considered first-line options.
- Proton pump inhibitors
- Approximately 1/3 of patients are ‘PPI responsive’
- If an endoscopic biopsy confirms the presence of eosinophils, then a trial of 8 weeks of a PPI can be undertaken
- After the 8-week trial, a repeat endoscopy and biopsy should be performed to look for persistent eosinophils
- The 1/3 of patients that respond to PPIs are diagnosed with ‘PPI responsive oesophageal eosinophilia
- If there is no resolution, a diagnosis of ‘true eosinophilic oesophagitis’ is made.
- Dietary manipulation
Dietary manipulation can be effective in both children and adults. It can be used as an initial treatment or as an adjunct to pharmacological therapy. The six most commonly implicated food groups are cow’s milk, wheat, egg, soy, peanut/tree nut, fish/shellfish. There are four main approaches:
- Elemental diet: this involves taking an amino acid mixture for six weeks. The mixture is often considered unpalatable, and compliance is often poor, but considerable improvement in symptoms and the histological picture has been noted. This will resolve symptoms in >90% though.
- Six food elimination diet (SFED) – exclusion of the six food groups listed above. Remission seen in >70%.
- Four food elimination diet (FFED) – uses the same principle but patients are allowed to eat nuts and fish/shellfish. Remission seen in >50%.
- Step-up approach – starts with just milk and wheat exclusion, then steps up to the FFED and then the SFED if unsuccessful. Remission seen in around 40% initially.
- Topical corticosteroids
Patients can also swallow ‘inhaled’ corticosteroids, e.g. fluticasone or aqueous nebuliser solutions (e.g. budesonide mixed with a sugary syrup). This coats the oesophagus with the corticosteroid without risking the side effects of taking oral corticosteroids. 50-80% will have histological remission with this strategy. Oral candidiasis is a significant problem, with around 30% suffering this side effect.
Prognosis of eosinophilic oesophagitis
Eosinophilic oesophagitis is a chronic condition that causes inflammation of the oesophagus and is associated with several potential complications, including:
- Oesophageal remodelling
- Fibrosis
- Stricture formation
There is no association with cancer, and no cases of associated oesophageal malignancy have been reported.
Remission is common, and continued maintenance therapy with topical steroids and/or dietary manipulation is advised.
Header image used on licence from Shutterstock.
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this article.