Wound healing, as a normal biological process in the human body, is achieved through four precisely and highly programmed events: haemostasis, inflammation, proliferation, and remodelling. For a wound to heal successfully, all four phases must occur in the proper sequence and time frame.
Haemostasis
After a wound occurs, the first stage in the healing process is haemostasis. Haemostasis is the process by which bleeding is controlled. It consists of three components:
- Primary haemostasis
- Secondary haemostasis
- Fibrinolysis
Primary haemostasis consists of local vasoconstriction, which reduces blood flow to the site of injury, and platelet plug formation. Vasoconstriction occurs due to smooth muscle contraction and is mediated by local reflexes and the release of thromboxane A2 and serotonin by activated platelets.
Platelets are always the first cells to be present in a wound. Their primary role is to form a platelet plug and to begin the process of creating an extracellular matrix that will secure the cellular components needed for wound healing to the surface of the wound. Platelets also release cytokines, such as platelet-derived growth factor, to attract inflammatory cells to the site of the wound.
Injury to a vessel wall results in the loss of endothelium and exposure of subendothelial collagen. The damaged endothelial cells release von Willebrand factor, which is necessary for platelet adhesion, and platelets adhere to the damaged area. Tissue thromboplastin is also released, which activates the intrinsic pathway of coagulation (see secondary haemostasis below).
Simultaneously, platelet granules release ADP, which initiates platelet aggregation. Thromboxane A2 is produced from arachidonic acid released from platelet phospholipids, which further induces ADP release, causing further aggregation and the formation of the platelet plug.
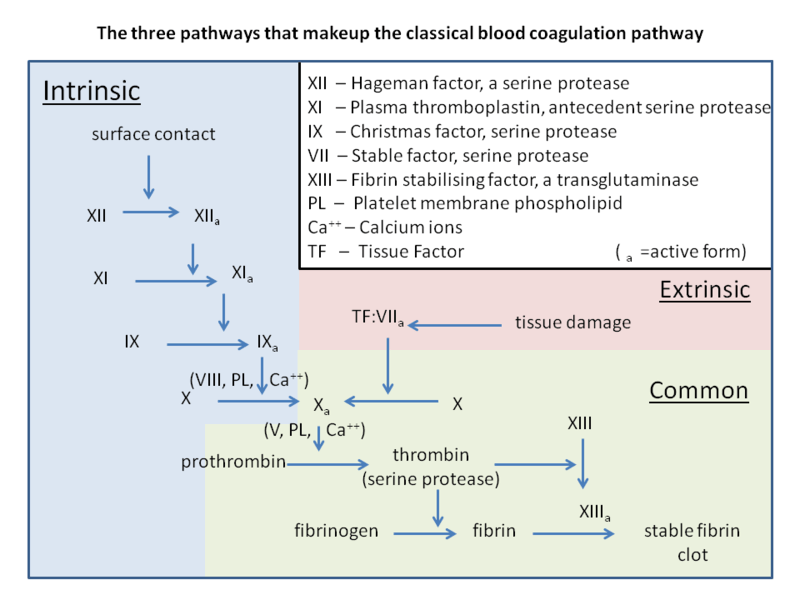
Once the platelet plug has been formed, secondary haemostasis occurs. In secondary haemostasis, clotting factors are activated in a sequence of events known as the ‘coagulation cascade’. The clotting cascade consists of three distinct pathways:
- The intrinsic pathway
- The extrinsic pathway
- The common pathway
The intrinsic pathway involves normal blood components, whilst the extrinsic pathway requires tissue thromboplastin, released by damaged cells. Both of these pathways result in the activation of factor X, which commences the final, common pathway. The end-point of the coagulation cascade is the conversion of soluble fibrinogen to insoluble fibrin by thrombin. A fibrin mesh is formed around the platelet plug, stabilising it and forming a ‘thrombus’ or ‘clot’.
Fibrinolysis is the process that prevents these clots from growing and becoming problematic. Fibrin is broken down into soluble fibrin degradation products by plasmin during the repair process in blood vessels and healing wounds.
The three phases of wound healing
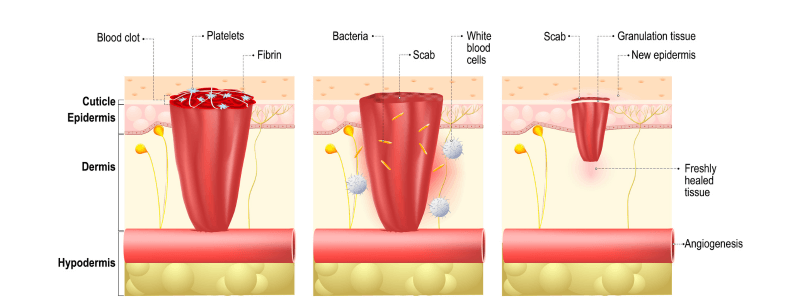
Following haemostasis, there are three phases of wound healing:
- The inflammatory phase (up to 48 hours after injury) – Blood vessels dilate to allow antibodies, white blood cells, growth factors, enzymes and nutrients to reach the wounded area. The characteristic signs of inflammation are seen. The predominant cell types seen are neutrophils and macrophages, which serve to autolyse devitalised necrotic tissue.
- The proliferative phase (up to 3 weeks after injury) – New granulation tissue, comprised of collagen and extracellular matrix, develops. Epithelialisation occurs during this phase. During epithelialisation, epithelial cells develop at the wound margins and then divide and migrate towards the centre of the wound. Angiogenesis occurs with fibroblasts and capillaries growing into the necrotic areas. Healing wound mass is greatest after three weeks.
- The maturation phase (up to 1 year after injury) – The final phase occurs when the wound has closed. This phase involves the remodelling of collagen from type I to type III. Cellular activity reduces, and the number of blood vessels in the wounded area regresses and decreases. Wound remodelling continues for up to 1 year.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcemexamprep.net for this article.






Informative writing regarding wound healing as i ever read.